This study aimed to explore the impact of bladder volume and compliance on BWT measurements in children with neurogenic bladder dysfunction, seeking to refine non-invasive diagnostic approaches.
This prospective study encompassed 50 children with spina bifida undergoing clean intermittent catheterization (CIC) and who had recent urodynamic testing as part of the standard of care. Participants were classified into normocompliant (NC; n=21) and low-compliant (LC; n=29) groups based on urodynamics outcomes.
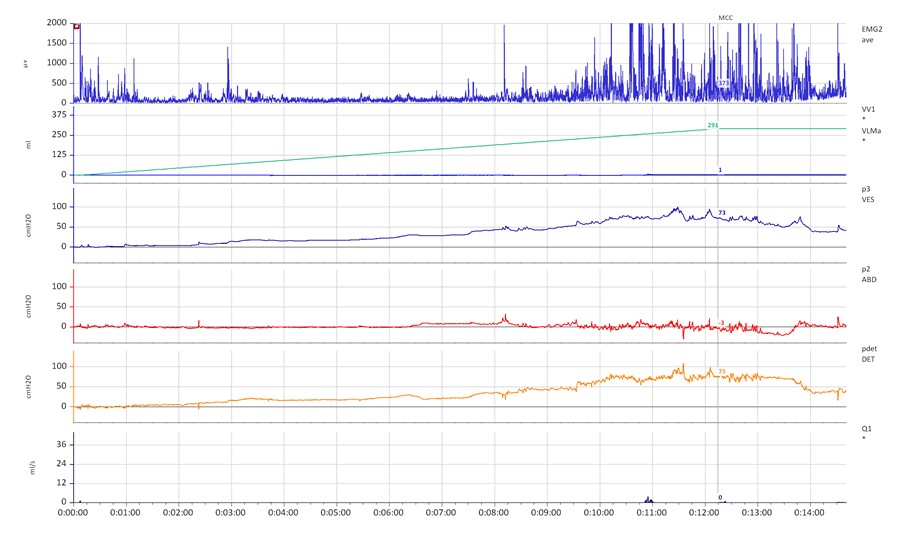
Figure 1. Typical urodynamic appearance of a low compliant bladder.
BWT was measured with ultrasound at various bladder volumes (full, half, and empty) across the various bladder walls.
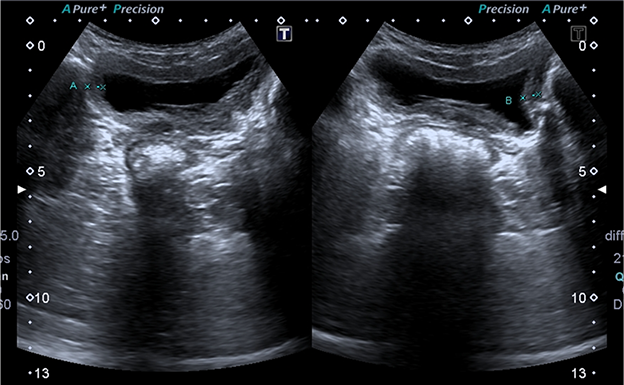
Figure 2. Ultrasonographic view of increased bladder wall thickness in a patient with neurogenic bladder dysfunction.
Significant increases in BWT were observed with decreasing bladder volumes across all measurements. The strongest association between BWT was observed in the anterior wall, demonstrating a slight inverse relationship (p=0.049, r=-0.280). These findings underscore the variability of BWT in response to bladder volume and compliance, highlighting the anterior wall's sensitivity to volume changes.
Nonetheless, when the bladder was fully expanded, measurements of the mean ± SD lateral wall thickness were notably greater in patients with low compliance (right: 2.18 ± 1.35 mm; left: 2.02 ± 1.4 mm) compared to those with normal compliance (right: 1.58 ± 0.68 mm; left: 1.45 ± 0.44 mm), with p=0.044 and p=0.033 for the right and left sides, respectively. This suggests altered bladder wall properties in the presence of reduced compliance.
The study revealed that lateral wall BWT measurements at full bladder volume are more indicative of bladder compliance states in children with neurogenic bladder dysfunction. This insight advocates for a nuanced approach to BWT measurement, favoring lateral wall assessments in cases of known or suspected low compliance. As the first study to concurrently evaluate bladder compliance and BWT ultrasonographically in this population, these findings pave the way for enhanced non-invasive diagnostic protocols.
Written by: Sabriye Gülçin Bozbeyoğlu,1 Furkan Ersoy,2 Arzu Canmemiş,3 Narmina Khanmammadova,4 Şeyhmus Kerem Özel 5
- Istanbul Goztepe Prof. Dr. Suleymands Yalcin City Hospital, Department of Radiology, Eğitim Mah Fahrettin Kerim Gökay Caddesi Kadıköy, Istanbul, Turkey.
- Istanbul Medeniyet University Goztepe Prof. Dr. Suleyman Yalcin City Hospital, Department of Pediatric Surgery, Eğitim Mah Fahrettin Kerim Gökay Caddesi Kadıköy, Istanbul, Turkey.
- Istanbul Goztepe Prof. Dr. Suleyman Yalcin City Hospital, Department of Pediatric Urology, Eğitim Mah Fahrettin Kerim Gökay Caddesi Kadıköy, Istanbul, Turkey
- Istanbul Medeniyet University Goztepe Prof. Dr. Suleyman Yalcin City Hospital, Medical School, Eğitim Mah Fahrettin Kerim Gökay Caddesi Kadıköy, Istanbul, Turkey.
- Istanbul Medeniyet University Goztepe Prof. Dr. Suleyman Yalcin City Hospital, Department of Pediatric Surgery, Eğitim Mah Fahrettin Kerim Gökay Caddesi Kadıköy, Istanbul, Turkey.


