Emphasis on Surgical Innovation
We highlight the growing popularity of laparoscopic procedures, particularly laparoscopic sacrocolpopexy (LSC), which demonstrates superior anatomical and subjective success rates compared to older techniques. This shift is vital, especially in light of complications associated with transvaginal mesh surgeries that have attracted significant regulatory scrutiny. By advocating for laparoscopic methods, the authors underscore an essential evolution in surgical practices aimed at enhancing patient safety and outcomes.
Training and Accessibility
The call for integrating laparoscopic techniques into urogynecology training is particularly noteworthy. As the field evolves, attracting new gynecologists is crucial for maintaining expertise and advancing care. Training in these modern techniques not only enhances the skill set of young professionals but also ensures that patients have access to the most effective and least invasive treatment options available.
Patient-Centric Approach
The article promotes a patient-centric philosophy in managing POP, acknowledging that each case is unique. The diversity of laparoscopic options available allows for personalized treatment plans that cater to varying degrees of prolapse, patient age, and health status. This tailored approach is vital for achieving higher satisfaction rates and improving patients' quality of life, which should be the primary goal of any medical intervention.
Evidence-Based Practice
The article presents a range of clinical outcomes associated with different laparoscopic techniques, emphasizing the importance of evidence-based practice. By providing data on success rates and complications, it supports the idea that adopting these techniques can lead to improved results. However, it also raises the question of whether further comparative studies are needed to solidify these claims and guide surgical decisions.
Future Directions in Women’s Health
The conclusion suggests a broader impact of laparoscopic techniques on the field of obstetrics and gynecology. This forward-thinking perspective is encouraging, as it implies that advancements in one area can lead to improvements across various aspects of women’s health. As more gynecologists become proficient in laparoscopic techniques, the potential for comprehensive enhancements in surgical care is significant.
Overview of Laparoscopic Techniques for POP Surgery
Laparoscopic Sacrocolpopexy (LSC)
LSC is the most recognized laparoscopic procedure for POP repair. It involves fixing the vaginal apex to the sacral promontory (L5-S1) using mesh, making it ideal for patients wishing to preserve their uterus. LSC has shown remarkable success rates, with an anatomical success rate of 96.9% and a subjective success rate of 94.1% based on a sample of 2,180 patients. However, the procedure's technical demands require advanced dissection and suturing skills.
Figure 1. Sacrocolpopexy is a surgical procedure that lifts your pelvic organs back into place using surgical mesh.1
Laparoscopic Lateral Suspension (LLS)
For cases where promontory fixation is challenging, laparoscopic lateral suspension (LLS) serves as a valuable alternative. This technique secures mesh arms to the abdominal wall, demonstrating favorable outcomes, with 78.4% of patients reporting symptom relief after one year. While both LSC and LLS yield high satisfaction rates, further comparative studies are necessary to establish their relative efficacy.
Figure 2. Anatomical positioning of the mesh after LLS. Reticulated area represents the mesh. Red point indicates a 5-mm skin incision.2
Laparoscopic Pectopexy
Laparoscopic pectopexy involves fixing mesh to the iliopectineal ligament, minimizing complications associated with sacrocolpopexy. Research indicates that pectopexy is as effective as LSC and has a notably lower incidence of postoperative constipation, making it an attractive option for patients with recurrent POP or previous mesh procedure failures.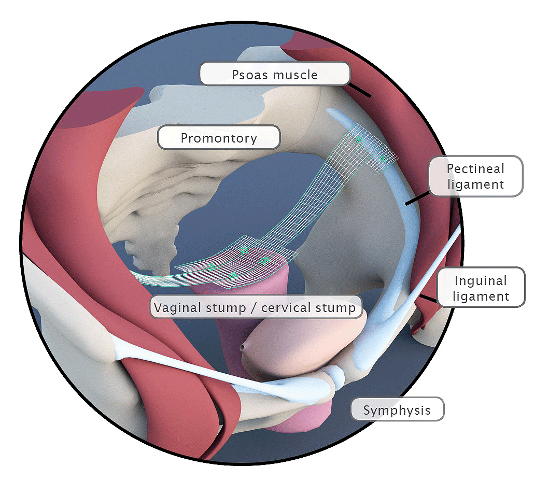
Figure 3. Bilateral Fixation on the Pectineal Ligament. Apical mesh repair following hysterectomy.
Laparoscopic Sacrospinous Ligament Fixation (LSSLF)
LSSLF secures the sacrospinous ligament using mesh. While effective, this approach requires meticulous dissection and carries a risk of bleeding. Although not widely established, LSSLF remains a viable option in select cases.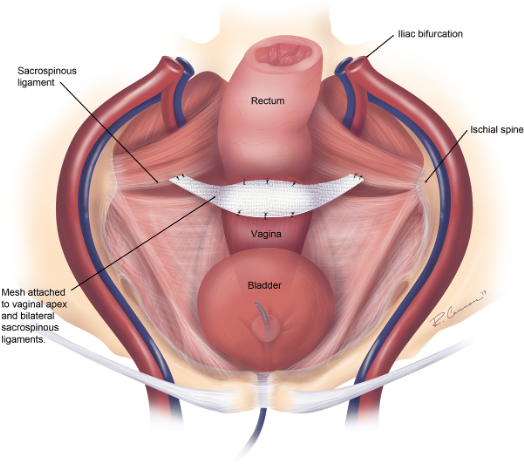
Figure 4. Laparoscopic Sacrospinous Ligament Fixations
Laparoscopic Native Tissue Repair (LNTR)
For patients preferring to avoid mesh, laparoscopic native tissue repair (LNTR) utilizes the body's own tissues for fixation. Recent studies suggest LNTR is comparable to conventional methods in terms of safety and effectiveness, though its lower tensile strength may increase the risk of recurrence.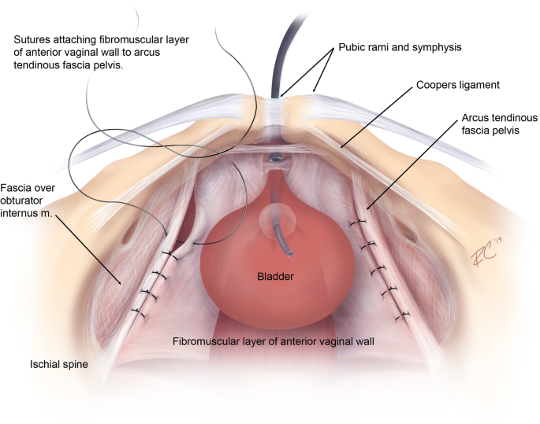
Figure 5. Laparoscopic Paravaginal repair3
Combined Approaches: LSC with Laparoscopic Ventral Rectopexy
Combining LSC with laparoscopic ventral rectopexy (LSC + LVR) effectively addresses patients with concurrent rectal prolapse, improving both anatomical and functional outcomes.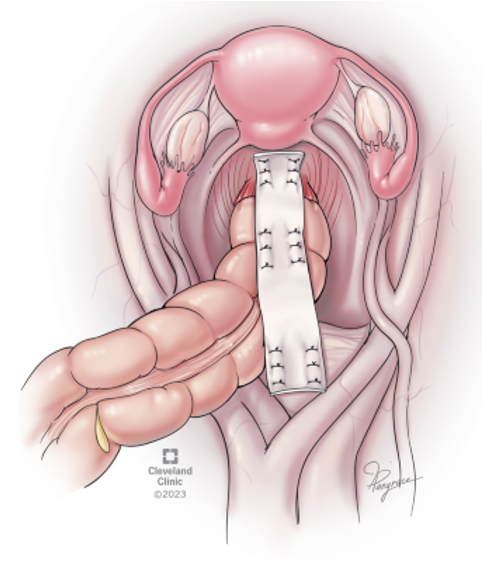
Figure 6. Anatomical scheme for ventral mesh rectopexy4
Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES)
The innovative vNOTES technique has gained traction as a minimally invasive option for POP repair. By accessing the peritoneal cavity through the vagina, this method combines the benefits of laparoscopic and vaginal surgery, presenting a promising alternative for suitable patients.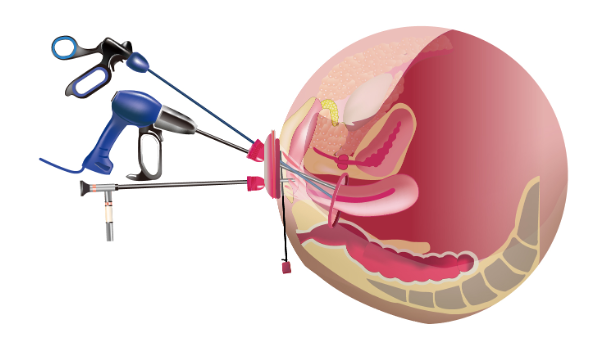
Figure 7. Vaginal Natural Orifice Transluminal Endoscopic Surgery
Robotic-Assisted Laparoscopic Procedures
Robotic-assisted laparoscopic techniques are emerging as a refined method for POP repair. Although current evidence does not conclusively favor robotic procedures over conventional laparoscopic techniques, their precision, and enhanced visualization may offer advantages in complex cases.
Conclusion
The diversity of laparoscopic techniques for treating pelvic organ prolapse underscores the need for individualized patient care. Each patient presents unique anatomical and health considerations, making it crucial to select the most appropriate surgical approach. By embracing these advanced laparoscopic methods, gynecologists can significantly improve treatment options, leading to enhanced patient outcomes and satisfaction. As these techniques gain wider acceptance, they hold the potential to revolutionize obstetrics and gynecology, ultimately benefiting women's health on a global scale.
Written by: Antonette Pesebre, MD, FPOGS, Urogynecology Center, Kameda Medical Center, Chiba, Japan
References:
- Cleveland Clinic. (2024). Sacrocolpopexy. https://my.clevelandclinic.org/health/treatments/17939-sacrocolpopexy.
- Okada Y, Hayashi T, Sawada Y, Tokiwa S, Yoshio Y, Gonocruz SG, Kitagawa Y, Nomura J. Laparoscopic lateral suspension for pelvic organ prolapse in a case with difficulty in performing laparoscopic sacrocolpopexy. IJU Case Rep. 2019 Mar 20;2(3):118-120.
- Developed by the Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. Joint report on terminology for surgical procedures to treat pelvic organ prolapse. Int Urogynecol J 31, 429–463 (2020). https://doi.org/10.1007/s00192-020-04236-1.
- Schabl, L., Hull, T., Erozkan, K. et al. Ventral mesh rectopexy for recurrent rectal prolapse after Altemeier perineal proctosigmoidectomy: feasibility and outcomes. Langenbecks Arch Surg 409, 49 (2024). https://doi.org/10.1007/s00423-024-03227-w.


