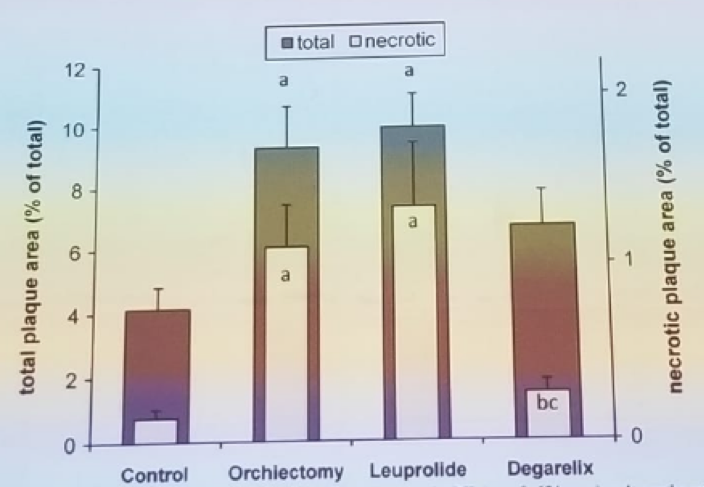
Figure 1: ADT induced (denovo) atherosclerosis:
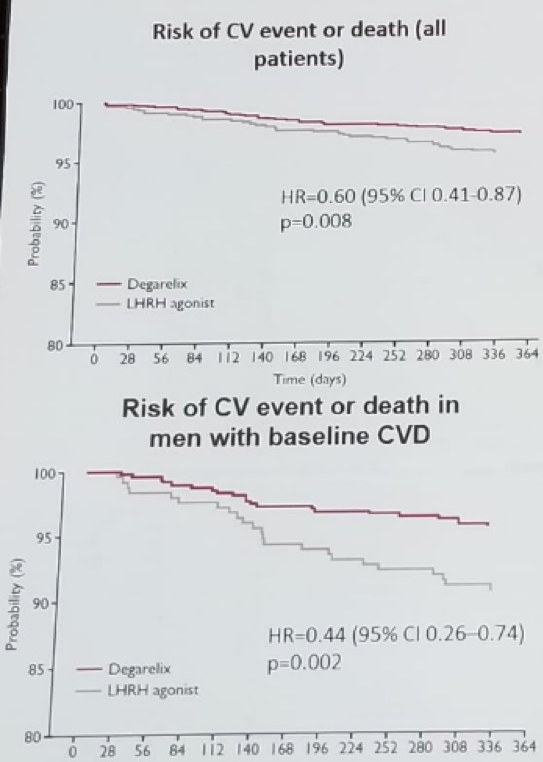
In a study comparing the risk of cardiovascular event or death between patients taking GnRH agonist and GnRH antagonists. Among men with prior cardiovascular disease, the 1-year event risk with GnRH antagonist was reduced compared with GnRH agonist (figure 2). 1
Figure 2 – Comparison of LHRH agonists and antagonists in the risk of a cardiovascular event:
In the macrophages surrounding the atherosclerotic plaque, there are receptors for Follicle stimulating hormone (FSH). These macrophages play a significant role in plaque formation and instability. In murine experiments, mice lacking the FSH receptors on the macrophages had considerably less atherosclerotic plaques and less necrotic areas. We can, therefore, assume, that the choice of ADT and its effect on FSH, have an impact on cardiovascular disease. It is known that LHRH agonists cause an initial increase in FSH levels, which later decreases. However, LHRH antagonists cause an immediate decrease in FSH secretion, which is much more significant than that caused by LHRH agonists.
There are two types of macrophages in the plaque surroundings:
M1 macrophages:
- Classically activated
- Pro-inflammatory
- pro-atherogenic
- Induce tissue injury and promote lesion development as well as enhances plaque vulnerability
2. M2 macrophages:
- Alternatively activated
- Anti-inflammatory
- Atheroprotective
- M2a – involved in tissue repair and can stabilize vulnerable plaques
- M2b and M2c – regulatory and anti-inflammatory and stabilize or even regress atherosclerotic plaques.
Therefore, the M2 macrophages are the more protective and beneficial macrophages. In murine models treated with GnRH antagonists, more intense staining of M2 macrophages was observed in the atherosclerotic plaque areas.
Pinthus concluded his interesting talk with some take-home messages. ADT induces obesity, metabolic syndrome, and atherosclerosis to a mode-specific extent. FSH levels may have a pivotal role in this effect. In patients with pre-existing atherosclerosis, ADT may induce plaque instability, through several mechanisms, including changes in macrophage plasticity, morphometrical changes: calcium deposition and tear, fibrous cap composition, and plaque hemorrhage.
References:
1. Albertsen PC, et al. Eur Urol 2014; 653: 565-73
Presented by: Jehonathan Pinthus, MD, McMaster University, Canada
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel


