- Age (life expectancy or follow-up time)
- Patient preference
- Cancer extent (clinical stage)
- Needle biopsy findings (grade, extent)
- PSA criteria (Total PSA and PSA density)
- Stage T1c
- Gleason score 6
- <3 cores involved by cancer
- No core with more than 50% involvement
- PSA density (PSA/gland weight) < 0.15
Figure 1 – Difference between Low risk and very low risk:
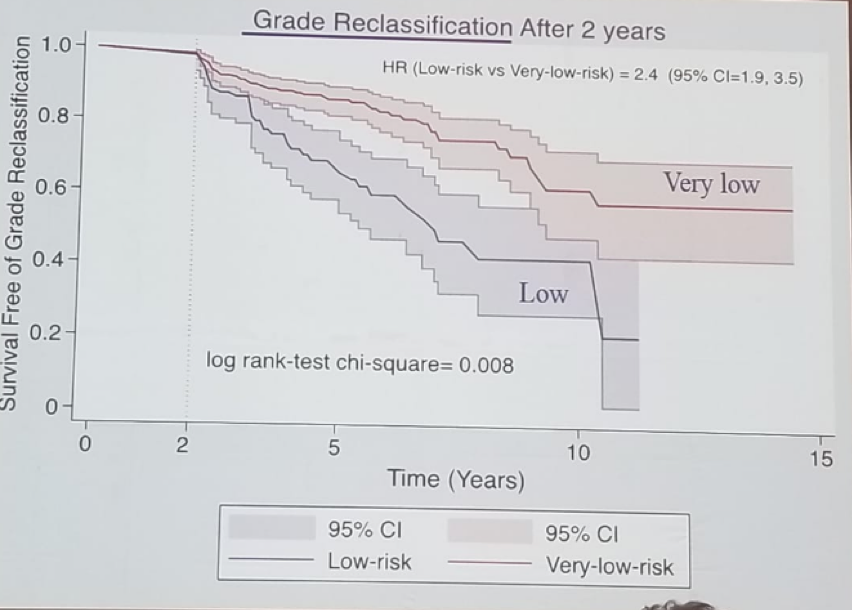
Later, the modified Epstein criteria were developed, including No Gleason pattern 4 or 5, less than 3 positive cores, unilateral cancer, and PSA density <0.15. The predictors of grade reclassification in men with favorable risk PC include diagnosed before 2005, increasing age, increasing PSA density, bilateral vs unilateral, risk status (Low risk vs. very low risk), and the total number of biopsies.
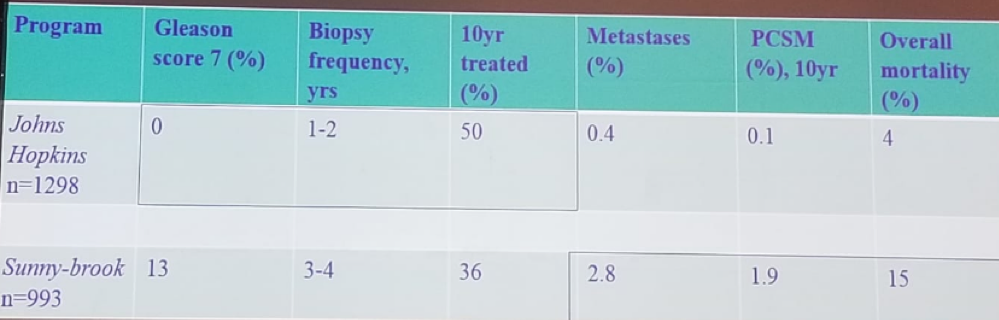
Depending on the criteria chosen, surveillance outcomes differ (Table 1). For Gleason 6 the 15-year metastases-free survival is 94%, while for Gleason 7 (3+4) it is 84%. According to the NCCN guidelines, AS for Gleason 7 should only be offered in the setting of a clinical trial.
Table 1 – Different surveillance criteria:
Epstein moved on to discuss novel biomarkers and imaging that may be useful in AS. These include urinary markers (PCA3, TMPRSS2:ERG), serum markers (PHI and 4K), molecular tissue based markers (prolaris, oncotype DX, PTEN), and multiparametric MRI.
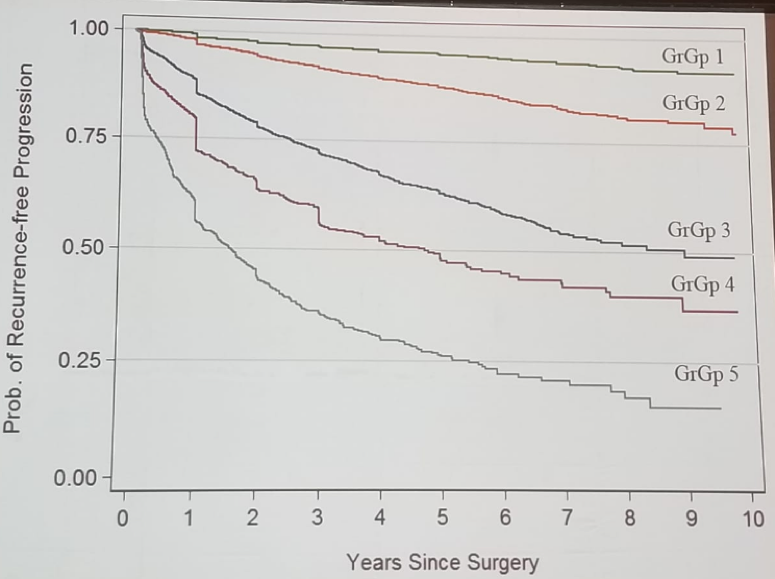
The last topic discussed was the formulation of the new grading of Gleason scoring system. Gleason 6 is the lowest grade reported although the score goes from 2-10. Patients are told they have a Gleason score of 6/10 and logically but incorrectly think that they have a tumor in the middle of the grade pectrum, contributing to the fear of cancer. Urologists need to reassure and educate patients when told they have a Gleason 6 cancer. The new grading system (Grade 1 – Gleason 3+3, Grade 2 – Gleason 3+4, Grade 3 – Gleason 4+3, Grade 4 – Gleason score 8, Grade 5- Gleason score 9-10), modifies how pathologists report PC to more accurately reflect their behavior (Figure 2). This new grading system has recently been accepted to the 2016 world health organization (WHO), college of American pathologists, and AJCC cancer staging manual – TNM system 8th edition.
Figure 2 – Difference between the new grading system:
Dr. Epstien summarized his talk stating that pathology plays a critical role in:
- Criteria for AS selection
- Criteria for intervention in AS
- Reporting PC to more accurately reflect extent and grade for both urologists and patients.
References:
1. Tosoian et al. J Urol 2013
2. Godtman et al. Eur Urol 2016
3. Mamawala MM. et al. BJU Int 2017
Presented by: Jonathan Epstein, MD, Johns Hopkins Medical Institutions, Baltimore, Maryland, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel


