The Massachusetts General Hospital (MGH) has a large AS cohort of 988 men from 1997 until 2014. The criteria for AS used in MGH include:
- Gleason <=6 (Gleason 3+4 in select patients with low volume disease)
- <=33% biopsy core positive
- <=20% cancer in any core
- PSA<10 ng/ml
In 2017, data had been published comparing 599 men starting AS at age <60, to 834 men starting AS over the age of 60.1 The study demonstrated no significant association between younger age and risk of definitive treatment or risk of biochemical recurrence after delayed surgery. Younger patient age was associated with decreased risk of biopsy-based Gleason score upgrade during AS but not with risk of definitive treatment in the intermediate term.
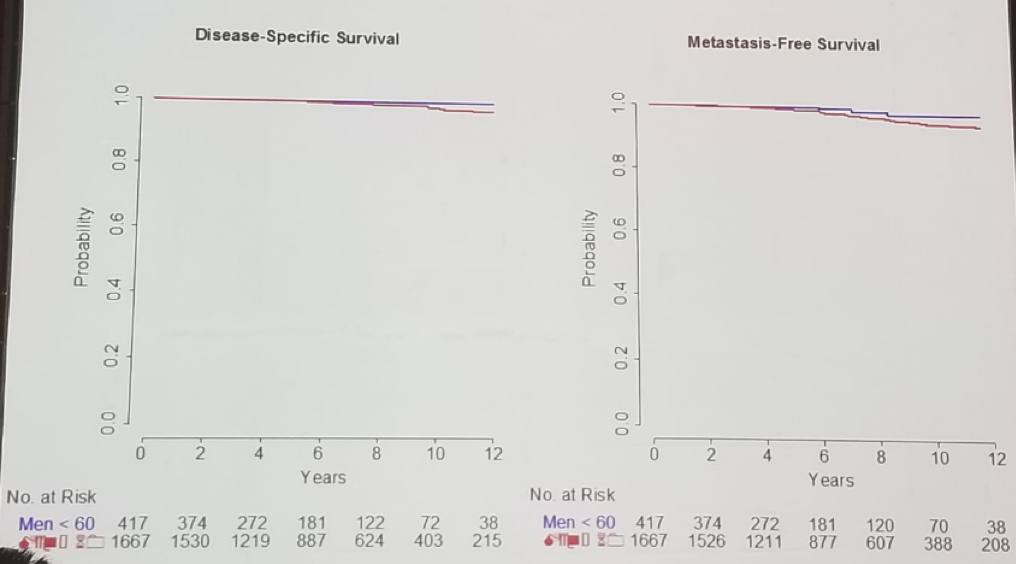
In 2016 collaboration with Dr. Laurence Klotz from Sunnybrook, Toronto, Canada began, with the purpose of assessing the outcomes of men who began AS at age under 60. The MGH and Sunnybrook combined analysis had 417 men younger 60 compared to 1667 men older than 60 starting AS. Freedom from treatment by age was not different among the age groups (Figure 1). Age<60 at diagnosis as a categorical variable was not a significant predictor of treatment in multivariable analysis. However, within those men diagnosed at age <60 age, age as a continuous variable was predictive of treatment on univariate analysis. Additional factors that were statistically significant at multivariable analysis included core involvement >20% vs. <20%, and PSA density >0.15 vs <0.15. Figure 2 demonstrates the disease-specific survival and metastasis-free survival in this study by age group.
Figure 1 – Freedom from treatment by age:
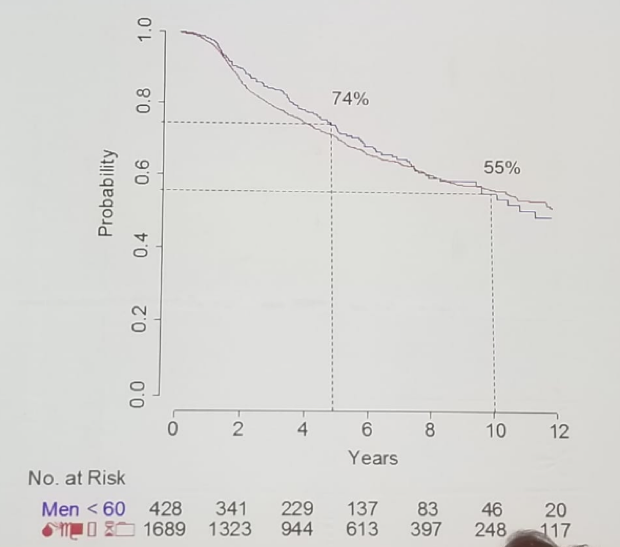
Figure 2 – Disease-specific survival and metastasis-free survival by age group:
Dr. Feldman summarized his talk with some important points:
- Men starting AS who are younger than 60 have lower risk disease.
- Freedom from treatment in appropriately selected men younger than 60 is similar to that in older men
- Younger men with higher volume disease and PSA density > 0.15 are more likely to progress on AS and require treatment
- Most men undergoing treatment do so for pathologic progression
- Most importantly, age < 60 should not be a contraindication to AS in appropriately selected men
References:
1. Leapman MS, et al. JCO 2017
Presented by: Adam Feldman, MD, Harvard Medical School, Boston, MA, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel


