We determined the sample number according to prevalence of OAB according to the following estimation: n = Z2P(1 - P)/d2, where Z = 1.96 (95% confidence level), P = 0.16 for expected OAB prevalence of 16% and d = 0.05 (10% confidence interval [CI] width). Based on this calculation, the minimum number was set at n = 195 participants. The research population comprised a convenient sample of university students. The women were randomly selected from two universities. In all, 7943 women completed a screening questionnaire with age, height, and weight information. Calculation of body mass index (BMI = m/h2, where m = body weight in kg and h = body height in m). All overweight women (BMI 25-29) were enrolled, with a total number of 1932. Of this number, every 7th woman was randomly selected, so a total of 276 women were examined.
The inclusion criteria were as follows: women aged 18-35 years; BMI 25-29, while The exclusion criteria were: stress urinary incontinence (SUI), surgery for gynecological or urological diseases, infection of the urinary tract, oncological or neurogenic disease of the lower urinary tract, incomplete questionnaires, and refusal to participate in the study.
They used the Voiding Diary, the Overactive Bladder Questionnaire (OAB-q), and the Incontinence Quality of Life (I-QOL) scale. Body composition was measured using direct segmental multi-frequency bioelectrical impedance analysis with body composition analyzer, with an assessment of skeletal muscle mass (kg), body fat mass (kg), body fat percentage (%), visceral fat area (cm2/level), and waist to hip ratio. Participants had OAB if they had urinary urgency, voiding eight or more times per day, two or more times per night, with or without urgency urinary incontinence.
There was 206 out of 276 women with an average age of 30.6±20.4 years, the response rate was 74.6%. Out of these, 102 were women with OAB and 104 without OAB. The voiding diary and OAB-q results confirmed OAB in 102 women. There was no significant difference in BMI between groups. The body composition analysis showed significant differences in body fat percentage, visceral fat area, and waist to hip ratio with significantly higher values in the OAB group (p < 0.01), skeletal muscle mass (kg), however, was significantly higher in the group without OAB (p < 0.01). Recorded I-QOL scores showed significantly worse parameters in total score in the OAB group (p < 0.001). Women with a fat percentage above 28% have a 1.95 times greater chance of developing OAB. Odds ratio [OR] = 1.95, (95% CI: 1.09-3.52, p = 0.024).
Table 1. Statistical comparison of monitored parameters in women with and without OAB
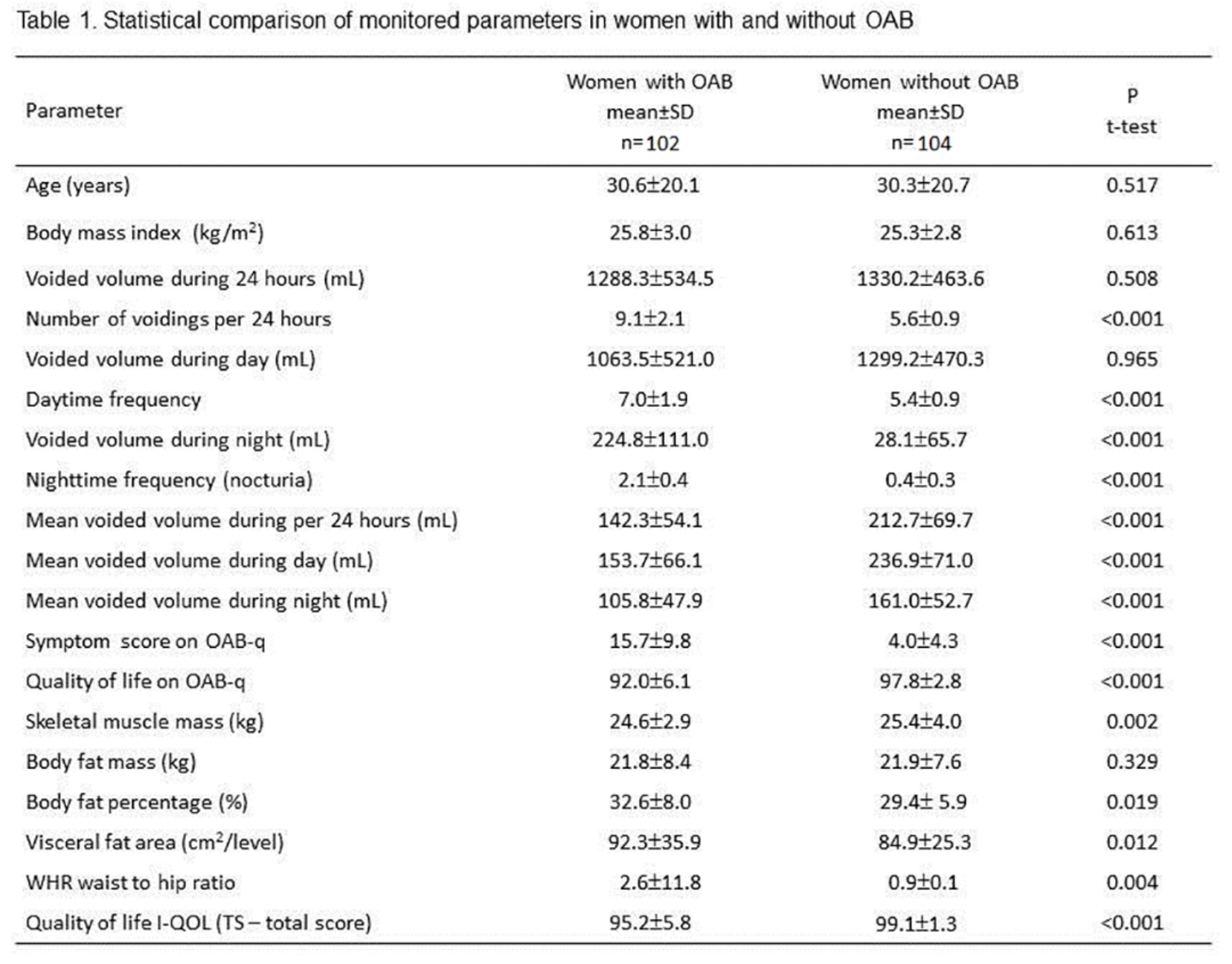
There was a higher value found in the OAB group for body fat percentage, visceral fat area, and waist to hip ratio with comparable BMI, confirming overweight by means of Body Composition Analysis. However, skeletal muscle mass was significantly higher in the non-OAB group. OAB has a negative impact on QoL. Data from two studies indicate, that measures of central adiposity are also correlated with urgency urinary incontinence.
They concluded that a higher body fat percentage, visceral fat area, and waist to hip ratio were significantly higher in overweight women with OAB, though comparable BMI. Women with a fat percentage more than 28 % have 1.95 greater likelihood of developing OAB.
Authors: Hagovská M1, Svihra J2, Bukova A3, Svihrova V4
Affiliations: 1. Department of Physiatry, Balneology, and Medical Rehabilitation, Faculty of Medicine, PJ Safarik University, Kosice, Slovak Republic, 2. Department of Urology, Jessenius Faculty of Medicine, Martin, Comenius University Bratislava, Slovak Republic, 3. Institute of Physical Education and Sport, PJ Safarik University, Kosice, Slovak Republic, 4. Department of Public Health, Jessenius Faculty of Medicine, Martin, Comenius University Bratislava, Slovak Republic
Written by: Bilal Farhan, MD; Clinical Instructor, Female Pelvic Medicine and Reconstructive Surgery, University of California, Irvine Medical Center, Twitter: @Bilalfarhan79 at the 2018 ICS International Continence Society Meeting - August 28 - 31, 2018 – Philadelphia, PA USA


