(UroToday.com) The 2022 Annual Meeting of the American Urological Association (AUA) was host to The International Bladder Cancer Group (IBCG) AUA Bladder Cancer Forum which featured a presentation by Dr. Patrick Hensley who was tasked with discussing the timing of radical cystectomy in BCG-unresponsive patients.
Dr. Hensley began his presentation by highlighting the current limitations in clinical staging accuracy. A series of 1,136 patients HGT1 patients treated with radical cystectomy demonstrated that almost half had T2 disease or worse, and there was lymph node involvement in 16.2% of cases.1 There are currently no prospective trials randomizing patients to novel bladder-sparing therapies versus standard of care radical cystectomy for patients with BCG-unresponsive non-muscle invasive bladder cancer (NMIBC).
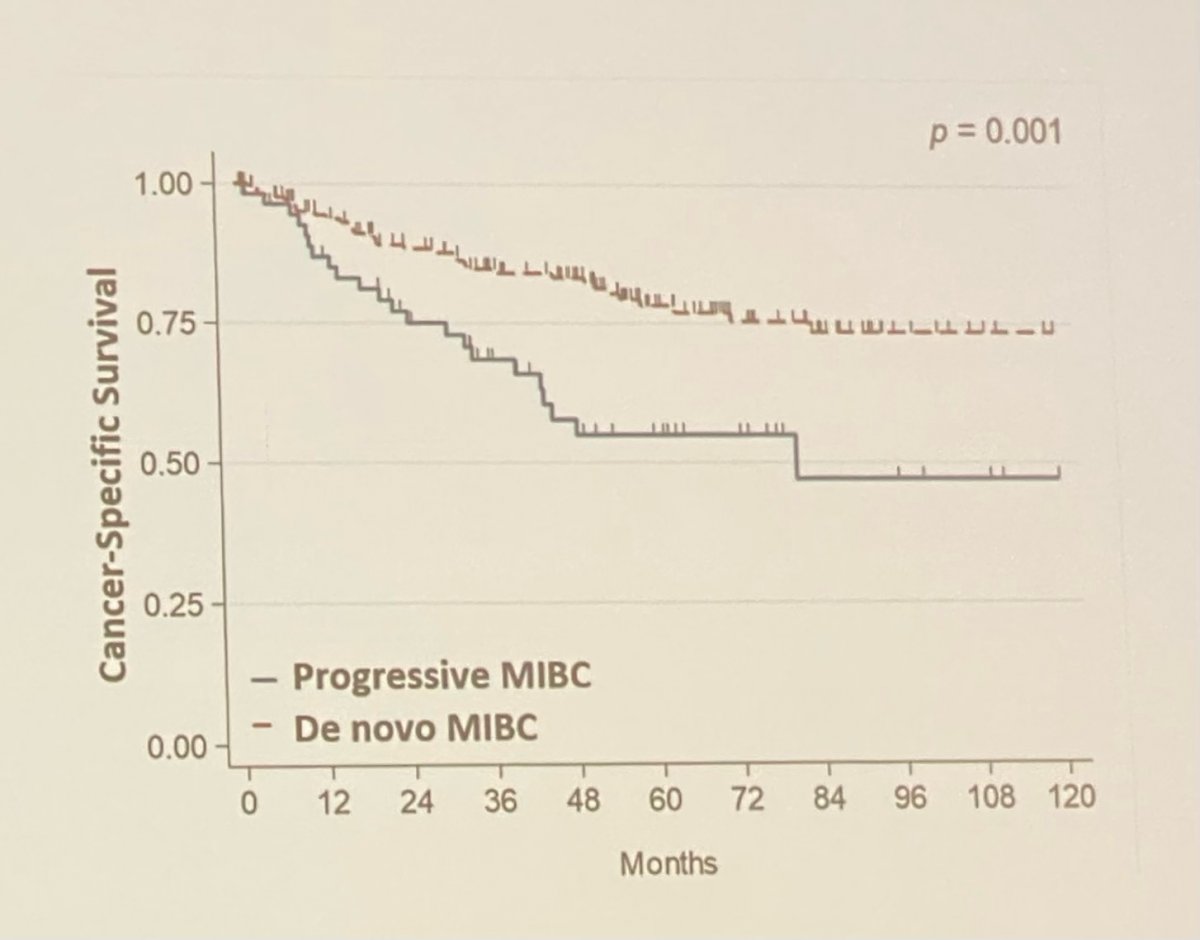
Hensley et al recently reported on results from the MD Anderson Cancer Center that demonstrated that patients with progressive cT2 disease or worse following BCG failure have significantly worse pathologic and survival outcomes compared to patients presenting with de novo muscle invasion.2
- Pathologic upgrading
- Progressive MIBC after BCG failure: 65%
- De novo MIBC: 43%
- Pathologic LN involvement
- Progressive MIBC after BCG failure: 28%
- De novo MIBC: 16%
Next, Dr. Hensley provided data from multiple contemporary series of radical cystectomy after salvage therapy. Looking at data from Keynote-057, the Nadofaragene trial, and the gem/doce series, the rate of salvage radical cystectomy was 16-40%, rate of pT2 disease or worse was 8-26%, and LN involvement was 3-12%. Looking at data from the MD Anderson Cancer Center series, specifically those with muscle invasion after BCG failure, the pT2 rate was 63%, nodal involvement was 27% and median OS was 4.1 years (compared to 9.5 years for those with pT1 disease undergoing RC following BCG failure). Clearly, there is a window of treatment that is missed once patients failing BCG progress to muscle invasion.
Does neoadjuvant chemotherapy have a role in the management of these patients? Based on data from the MD Anderson, it appears the answer is yes. Looking at CSS, patients with progressive MIBC had a median CSS of 52 months compared to 85 months for those with de novo MIBC when treated with radical cystectomy alone. Conversely, when both cohorts are treated with neoadjuvant chemotherapy, the median CSS improves to 91 months in the progressive MIBC group and 88 in the de novo group.
Dr. Hensley concluded his presentation with the following regarding paradigm improvement:
- We need to understand limitations of current clinical staging
- Develop predictive biomarkers “fit for purpose”
Presented by: Patrick Hensley, MD, Clinical Fellow, MD Anderson Cancer Center, Houston, TX
Written by: Rashid Sayyid, MD, MSc – Urology Chief Resident, Augusta University/Medical College of Georgia, @rksayyid on Twitter during the 2022 American Urological Association (AUA) Annual Meeting, New Orleans, LA, Fri, May 13 – Mon, May 16, 2022.
References:
- Fritsche H, Burger M, Svatek RS, et al. Characteristics and outcomes of patients with clinical T1 grade 3 urothelial carcinoma treated with radical cystectomy: results from an international cohort. Eur Urol. 2010;57(2):300-309.
- Hensley PJ, Bree KK, Campbell MT, et al. Progression of Disease after Bacillus Calmette-Guérin Therapy: Refining Patient Selection for Neoadjuvant Chemotherapy before Radical Cystectomy. J Urol. 2021;206(5):1258-1267.


