(UroToday.com) In a moderated poster presentation at the 2022 American Urologic Association Annual Meeting held in New Orleans and virtually, Dr. Okhaware presented results of a comparison of health care cost and utilization according to surgical approach (robotic versus laparoscopic) among patients undergoing partial and radial nephrectomy. In introducing this talk, Dr. Okhaware noted that there has been widespread adoption of robotic surgery for partial and radical nephrectomy without a strong evidentiary base. One of the major concerns regarding widespread uptake of robotic surgery is the associated costs. However, the cost of utilization remains an important factor that requires investigation without conclusive data to guide decision making. Thus, the authors sought to compare the cost and healthcare utilization one year after robotic-assisted surgery (RAS) to laparoscopic (LAP) surgery for radical (RN) and partial nephrectomy (PN).
To do so, the authors performed a retrospective cohort study of patients who underwent RN or PN for kidney cancer between 2013 and 2018 using IBM® MarketScan® Databases, a US commercial claims database. They considered a number of healthcare resource utilization related outcomes including length of stay and expenditure for index surgery, post-operative 1-year total healthcare expenditure, healthcare utilizations, and total missed days of work due to healthcare utilization. To account for baseline differences between patients undergoing robotic and laparoscopic surgery, the authors used inverse probability of treatment weighting (IPTW) based on baseline patient characteristics.
In their dataset, the authors identified 3,824 patients, of whom 2,008 had PN (1,263 RAS vs 745 LAP) and 1,816 had RN (456 RAS vs 1,360 LAP). Whether undergoing partial or radical nephrectomy, patients treated with robotic assisted surgery had statistically significantly lower index length of stay than those who underwent laparoscopic surgery (PN: 2.4 vs 2.6, p=0.004; and RN: 2.5 vs 2.9, p < 0.001), though the differences is of debatable clinical relevance. Further, those treated with robotic surgery had lower or comparable index expenditure versus those treated laparoscopically (PN: $29,258 vs $32,026, p=0.005; and RN: $30,342 vs $28,668, p=0.500).
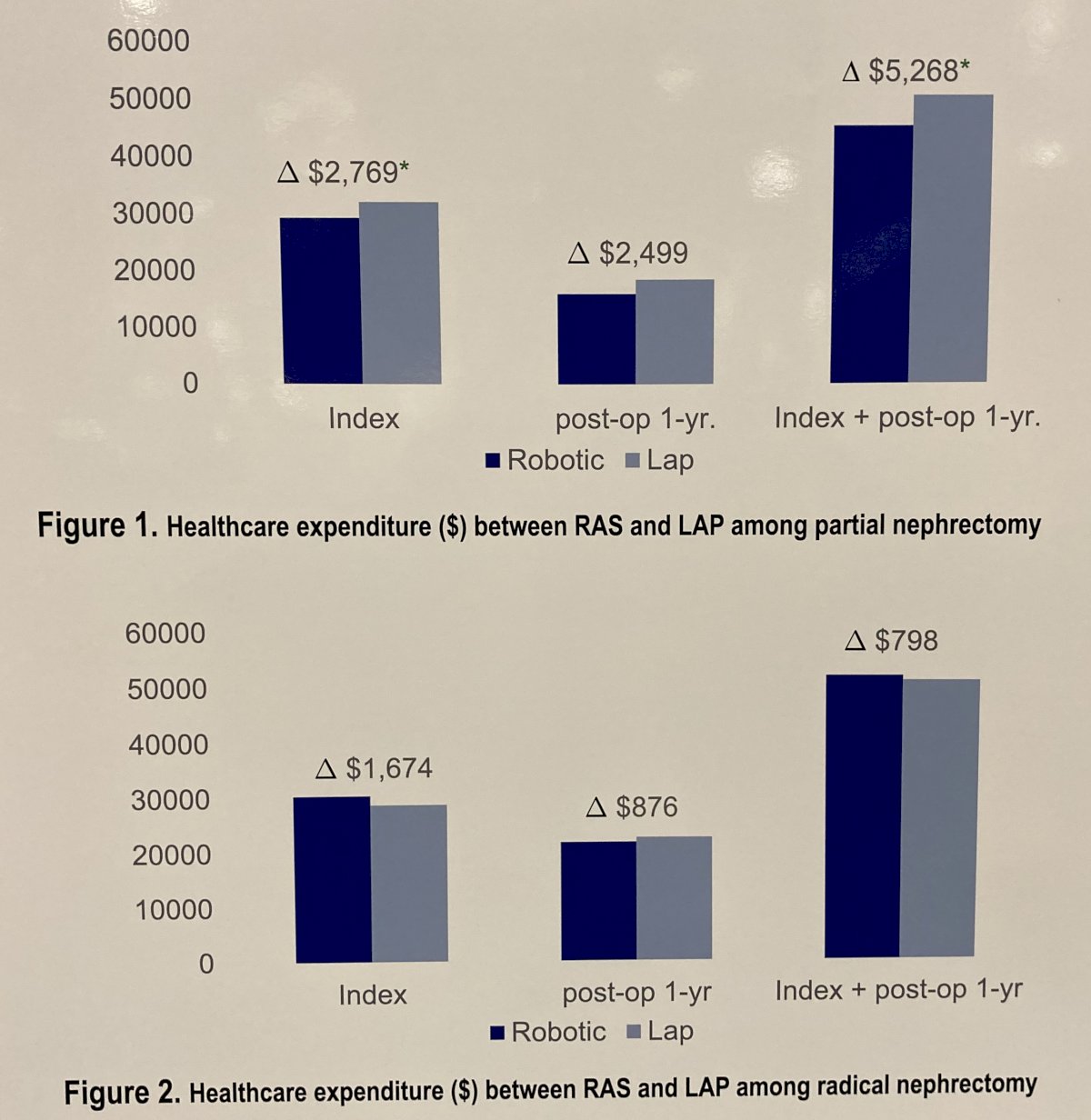
Additionally, 1-year total expenditures in the post-operative period were comparable between those undergoing robotic and laparoscopic surgery (PN: $16,010 vs. $18,509, p=0.070; and RN: $21,633 vs. $22,509, p=0.120). Of the same time period, patients who underwent robotic surgery had lower or comparable post-operative inpatient days (PN: 0.7 vs 0.9 days, p=0.032; and RN: 0.7 vs 0.7, p=0.230). Finally, no differences were found in terms of readmission, ER visits, outpatient visits, and post-operative missed workdays.
Thus, the authors conclude that, for partial and radical nephrectomy, robotic-assisted surgery has comparable health care utilization and total one-year post discharge cost to a laparoscopic approach. Further research is warranted to evaluate the impact of the surgical approach on post-operative kidney function and consequent economic burdens.
Presented by: Kennedy Erele Okhawere, MD, MPH – Icahn School of Medicine At Mount Sinai


