(UroToday.com) The 2022 American Urological Association (AUA) Annual Meeting included a session on the detection and screening of prostate cancer and a presentation by Dr. Michael Basin discussing disparities regarding shared decision-making in prostate cancer screening. Urologic prostate cancer screening guidelines universally recommend shared decision-making regarding PSA testing. The objective of this study presented by Dr. Basin and colleagues was to examine socio-demographic differences in shared decision-making for prostate cancer screening in the United States.
A retrospective cross-sectional study among men undergoing PSA screening was conducted using the 2018 National Health Interview Survey database in the United States. Outcomes included self-reported PSA testing and whether respondents had a discussion regarding its advantages with their healthcare provider. Multivariable logistic regression analyses were used to evaluate socio-demographic predictors of undergoing PSA screening and have a discussion regarding PSA testing advantages.
There were 118,859 men identified, 59,595 men aged 45-75, of which 5,605 (9.4%) answered questions regarding PSA testing and 5,632 (9.5%) answered questions regarding discussing the advantages and disadvantages of PSA screening. There were 39.5% of men that discussed the advantages and 25.6% of men that discussed the disadvantages of PSA testing.
The mean age of the cohort was 63.7 years (SD 10.8). 6,029 (81.5%) were white, 765 (10.3%) were black, and 603 (8.1%) were other or multiple races. On multivariable analysis, older (OR 1.08, 95% CI 1.07-1.09, p<0.001), black (OR 1.32, 95% CI 1.12-1.57, p=0.001), and homosexual (OR 1.70, 95% CI 1.22-2.24, p=0.002) men were significantly more likely to undergo PSA testing:
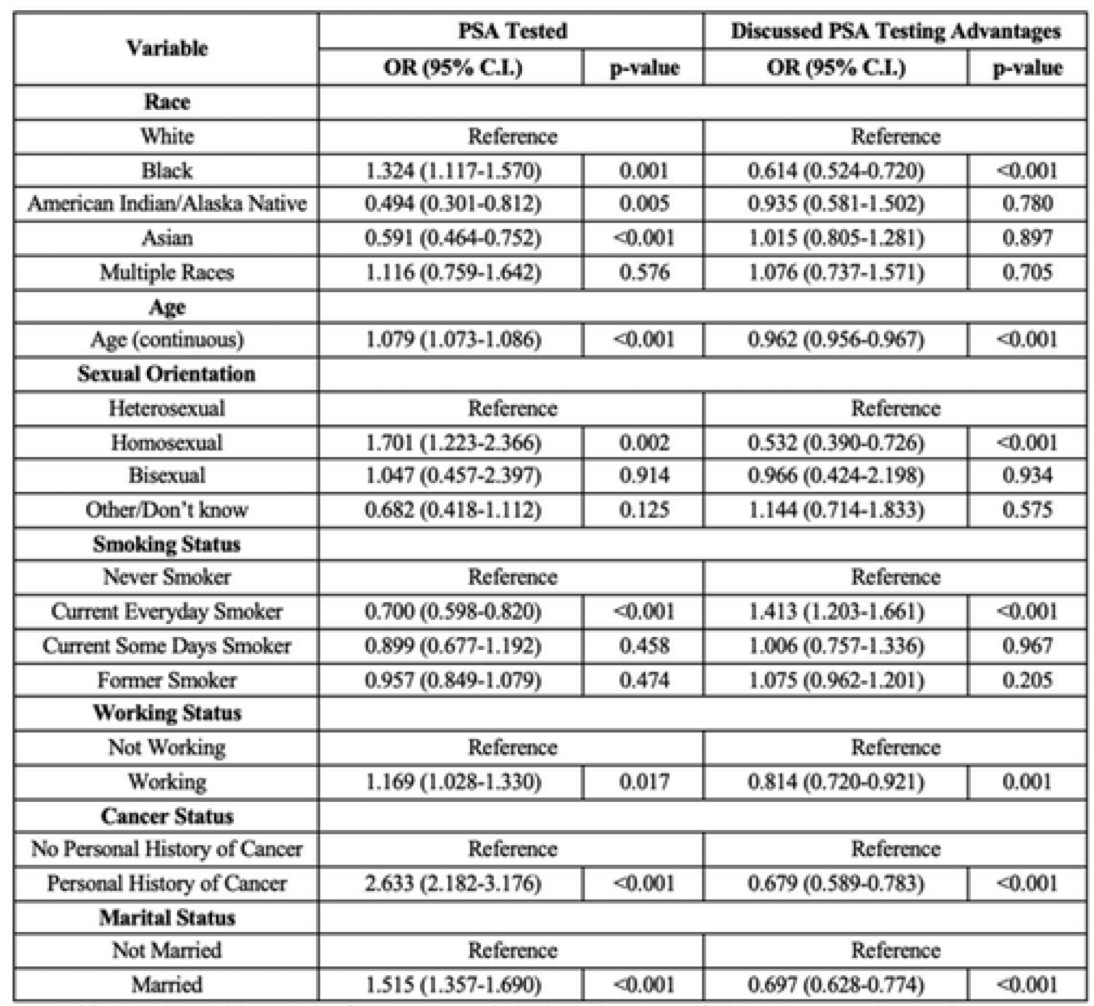
However, on multivariable analysis, the same group of older (OR 0.96; 95% CI 0.96-0.97, p<0.001), black (OR 0.61; 95% CI 0.52-0.72, p<0.001), and homosexual (OR 0.53; 95% CI 0.39-0.73, p<0.001) men were significantly less likely to have a discussion regarding PSA testing advantages.
Dr. Basin concluded his presentation by discussing disparities regarding shared decision-making in prostate cancer screening with the following take-home messages:
- Disparities exist in shared decision-making in prostate cancer screening
- Only about a third of men underwent discussion on PSA testing
- Older men and minorities, including black and homosexual men, were less likely to have a discussion regarding the advantages of PSA testing despite being more likely to undergo PSA testing
Presented by: Michael Basin, MD, SUNY-Upstate, Syracuse, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Urological Association (AUA) Annual Meeting, New Orleans, LA, Fri, May 13 – Mon, May 16, 2022.


