(UroToday.com) The 2024 South Central AUA annual meeting included a session on prostate cancer, featuring a presentation by Dr. Xiaosong Meng discussing focal therapy in prostate cancer. In 2024, there were an estimated 299,010 new cases of prostate cancer diagnosed in the United States, and of these new cases ~60-70% will be low to intermediate risk disease. Supported across multiple guidelines, there are various accepted treatment modalities for the different prostate cancer risk groups:
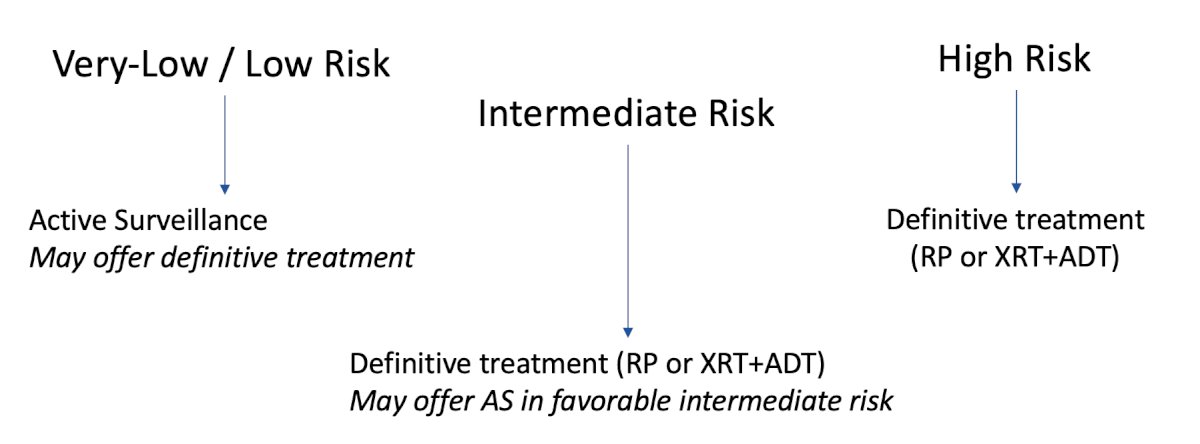
Treatment decisions are difficult with downsides of both definitive treatment and active surveillance. Downsides of definitive treatment include:
- Urinary incontinence
- Erectile dysfunction
- Adverse effects of hormonal therapy
- Bladder and bowel radiation toxicity
Downsides of active surveillance include:
- Need for strict surveillance
- High rates of converting to definitive therapy: 40% at 5 years, 55% at 10 years, 60% at 15 years
- A higher risk of metastases compared to active treatment
- The psychological impact of active surveillance
Dr. Meng notes that perhaps focal therapy offers a third, middle of the road, option that is more aggressive than active surveillance, but not as drastic as definitive treatment. The aim of focal therapy is to maintain oncological of active treatment, and tissue-preservation to optimize function. Focal therapy may be lesion targeted, partial gland (less than hemi ablation), partial gland (more than hemi ablation), and subtotal ablation:
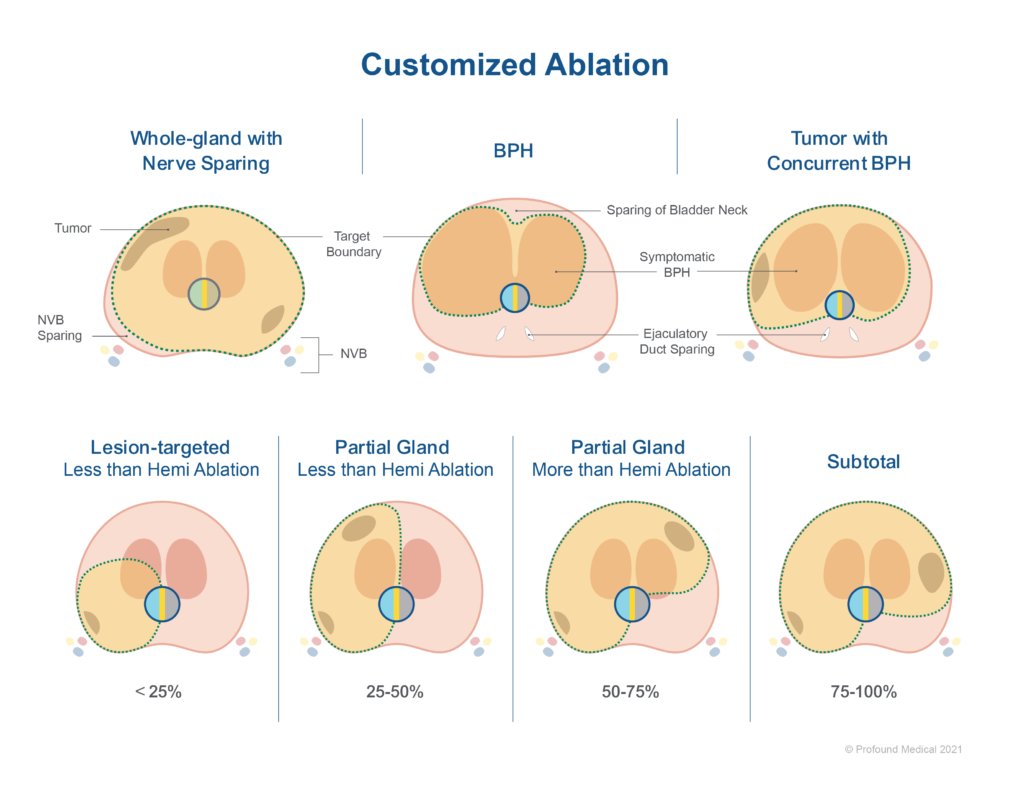
Dr. Meng emphasized that patient selection is critical for focal therapy. This includes the following criteria:
- A visible lesion on high quality multi-parametric MRI
- Targeted/systematic biopsy with concordant disease with imaging
- Willing to adhere to close follow up after treatment
- Select the proper ablation modality for the patient
- Based on consensus statements, patients should have organ-confirmed, intermediate risk disease, with a PSA < 20 ng/mL
There are several modalities of prostate cancer ablation. These using heat include: HIFU, TULSA, laser, radiofrequency ablation, microwave, and water vapor. Additionally, there is cryotherapy, radiation, and non-thermal options including irreversible electroporation, photodynamic therapy, and aqua-ablation. Moreover, there is considerations for how to access the prostate for ablation. This may include a natural orifice in the context of HIFU or TULSA, or a transperineal approach in the case of irreversible electroporation, cryotherapy, laser ablation, or HDR brachytherapy.
Cryoablation uses a fast freeze cycle with argon and a slow thawing cycle with helium. This leads to denaturation of cellular proteins, intracellular osmotic dehydration, and metabolic failure, with delayed vascular injury as the main mechanism of cell death. This occurs via a transperineal approach in combination with a urethral warming catheter:
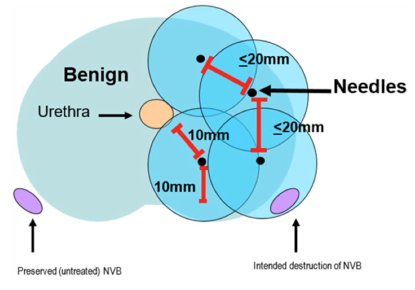
Cryotherapy is associated with biochemical recurrence free rates of 75-85%, urinary continence rates of 96-98%, and potency preservation rates of 60-80%.
HIFU uses thermal energy, which leads to tissue ablation by raising the temperature to over 60 degrees using focused high intensity ultrasound. Tissue ablation occurs from coagulative necrosis and internal cavitation:
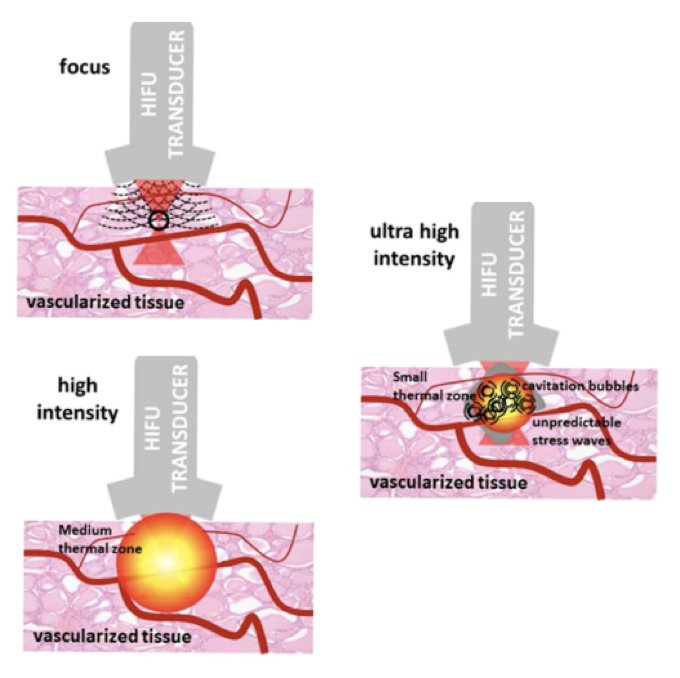
HIFU is associated with biochemical recurrence free rates of 78-85%, urinary continence rates of 97%, and potency preservation rates of 60-80%. The retreatment rate for HIFU is ~20-70%, with 19% having radical treatment at 8 years.
Irreversible electroporation uses high voltage low energy electric pulses that travel between two or more electrodes, causing permanent changes to the cell membrane and apoptosis:

Irreversible electroporation is associated with biochemical recurrence free rates of 69-91%, urinary continence rates of 98%, and potency preservation rates of 60-90%. Approximately 17% of patients require radical treatment over a median of 35 months after irreversible electroporation.
TULSA (transurethral ultrasound ablation of the prostate) is an outpatient procedure in an MRI suite under general anesthesia. This modality combines MRI imaging and thermography with high intensity ultrasonic energy to ablate prostate tissue, enabling a range of treatment from focal to whole gland therapy:

Among patients with mostly intermediate risk disease, at 1 year 80% of patients have no significant disease, however, at 5 years 21% of patients may have to undergo an additional intervention for prostate cancer.
Dr. Meng emphasized the importance of selecting the right modality for focal therapy, which depends on patient factors, such as BMI, prior surgeries (that may lead to a tight anal ring), and implants (such as hip implants or previously placed fiducial markers). It is also important to assess prostate anatomy, specifically the size of the gland, the distance from the energy source to the tumor and margins, the location of calcifications or cysts, and the possibility of anatomical distortions from prior TURP or focal therapy. Disease specific characteristics are also important, such as the tumor location (anterior, posterior, or apical), proximity of critical structures (rectum, sphincter, or neurovascular bundle), size of the tumor, and whether there is unilateral or bilateral disease.
Dr. Meng concluded his presentation by discussing focal therapy in prostate cancer with the following take-home points:
- Focal therapy is an important tool in our armamentarium for treating prostate cancer
- There are multiple energy sources available, but overall oncologic outcomes are similar
- Focal therapy allows good preservation of continence and decent preservation of potency
- There is significant patient interest in focal therapy options, but patient selection is critical
Presented by: Xiaosong Meng, MD, PhD, UT Southwestern Medical Center, Dallas, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 South Central American Urological Association (AUA) Annual Meeting, Colorado Springs, CO, Wed, Oct 30 – Sat, Nov 2, 2024.


