(UroToday.com) The 2024 South Central AUA annual meeting included a session on bladder cancer, featuring a presentation by Dr. Ali Nasrallah discussing the BRAVO study assessing white versus blue light cystoscopy in non muscle invasive bladder cancer (NMIBC) among veterans in an equal access setting. Bladder cancer is the 6th most common cancer in the United States, with 83,190 new cases expected in 2024. Recent studies have shown conflicting evidence regarding the utility and impact of blue light cystoscopy on oncologic outcomes such as recurrence.
Moreover, there is a lack of real world data on blue light cystoscopy oncologic outcomes. At the 2024 South Central AUA annual meeting, Dr. Nasrallah and colleagues described oncologic outcomes among a predominantly high-risk NMIBC patient cohort that underwent blue light cystoscopy versus white light cystoscopy in the Veterans Affairs (VA) Healthcare System, the largest equal access setting in the United States.
This study identified 740 NMIBC patients within the VA that underwent blue light cystoscopy or white light cystoscopy only from 1997 to 2021. A total of 348 blue light cystoscopy recipients were identified and then compared to 392 white light cystoscopy recipients using 1:1 propensity score matching (PSM):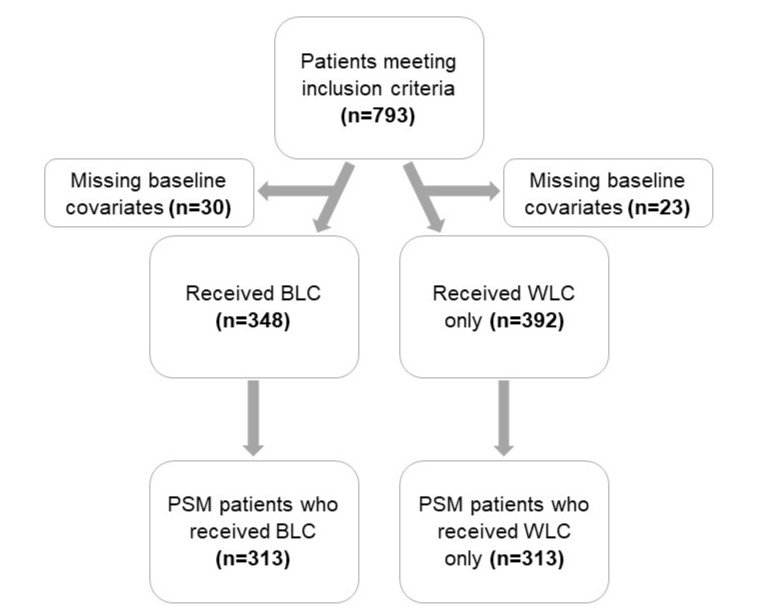
The distributions of age at diagnosis, year of diagnosis, sex, and ethnicity were balanced between the blue light cystoscopy and white light cystoscopy cohorts. The variables used to calculate the propensity score between the cohorts included patient race, location of bladder cancer diagnosis (VA vs outside VA), smoking status, and disease risk. Dr. Nasrallah and colleagues determined time to recurrence (censored at year-3), time to progression (censored at year-3), and overall survival following either blue light cystoscopy or white light cystoscopy from date of bladder cancer diagnosis using the Kaplan-Meier method and calculated the hazard ratio from Cox proportional hazards model adjusting for demographics and clinical characteristics.
The final cohort of 626 patients was comprised of 313 blue light cystoscopy and 313 white light cystoscopy recipients. The median age at diagnosis was 71 (IQR 65-76) years and 159 (25%) had bladder cancer recurrence. Compared to white light cystoscopy patients, blue light cystoscopy patients were significantly more likely to receive BCG therapy (61% vs 43%; p < 0.01) and intravesical therapy (48% vs 27%; p < 0.01):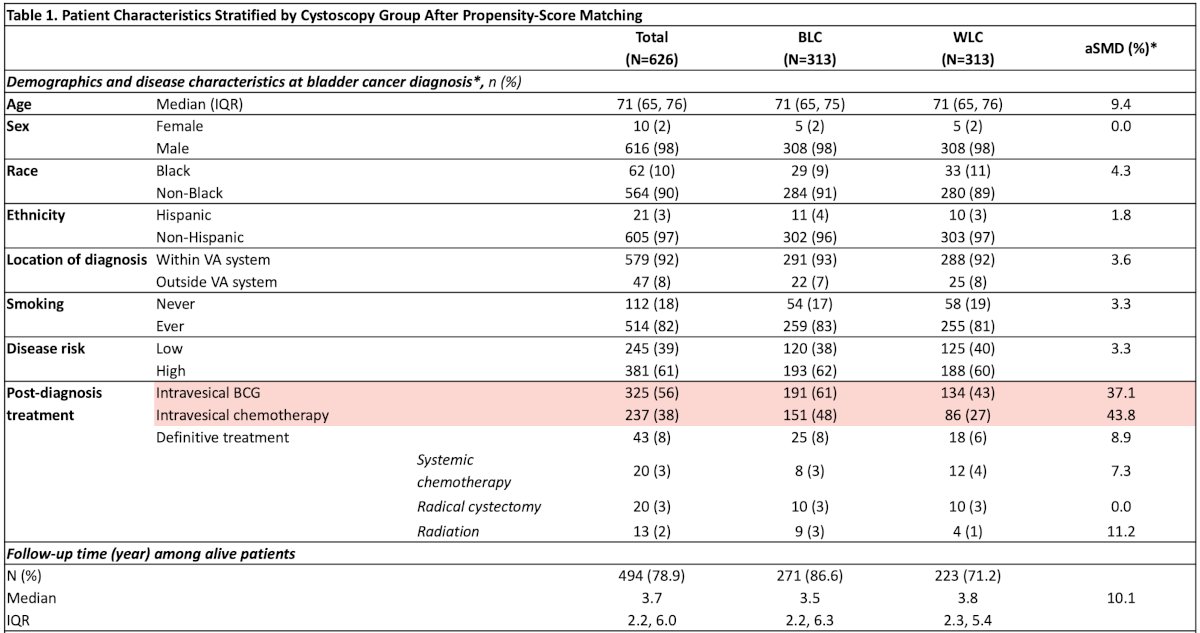
The median follow-up was 3.5 years (IQR 2.2 – 6.3) and 3.8 years (IQR 2.3 – 5.4) for the blue light cystoscopy and white light cystoscopy cohorts, respectively. Recurrence risk at 3-years was significantly reduced following blue light cystoscopy (75% vs 67%; HR 0.62, 95% CI 0.45-0.86), but progression risk at 3-years was comparable between the groups (38 cases; HR 0.71, 95% CI 0.37-1.38):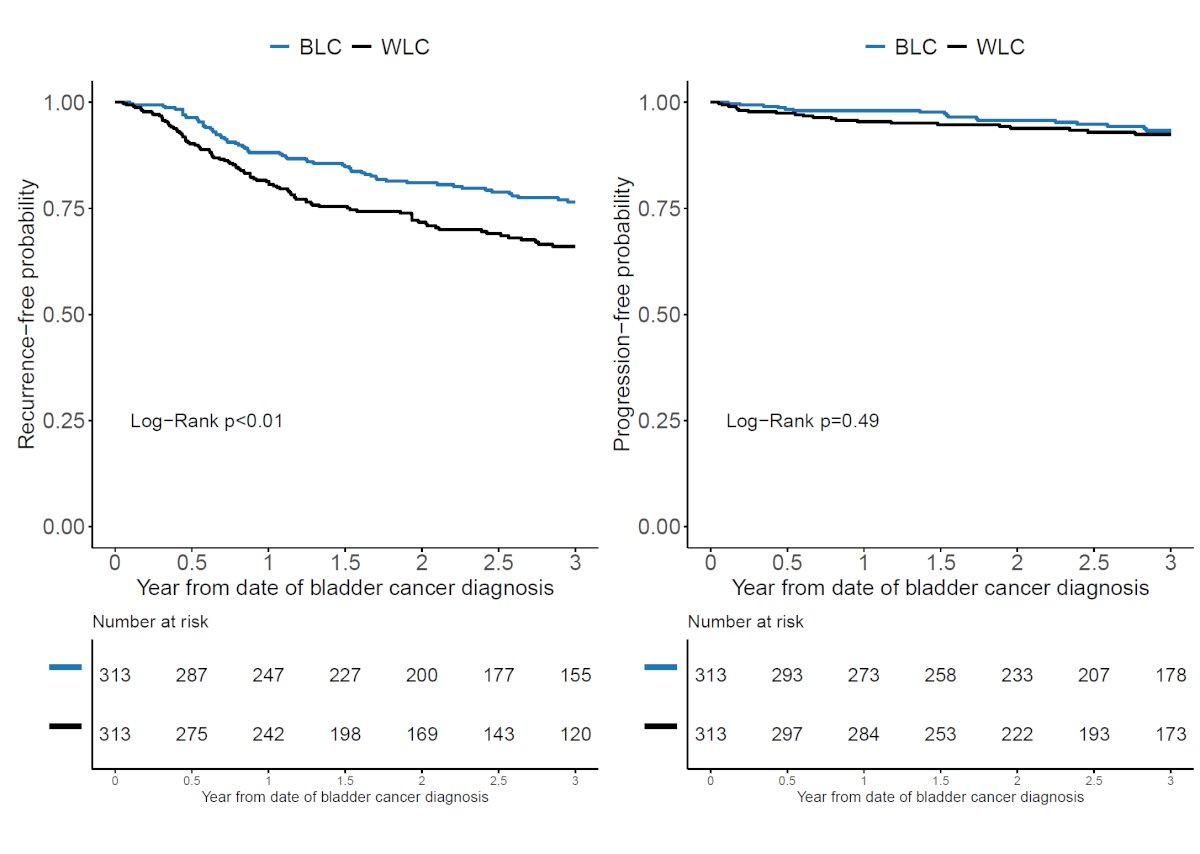
Dr. Nasrallah concluded his presentation discussing the BRAVO study assessing white versus blue light cystoscopy in NMIBC among veterans in an equal access setting with the following take-home points:
- In this PSM cohort study of NMIBC patients in an equal-access setting, the use of blue light cystoscopy was associated with reduced risk of disease recurrence
- Blue light cystoscopy was also associated with increased use of intravesical treatments, but with no difference in definitive treatment suggesting that perhaps blue light cystoscopy can assist in appropriately directing therapy
- These findings provide real world evidence for the oncologic benefits of utilizing blue light cystoscopy
Presented by: Ali Nasrallah, MD, The University of Texas Medical Branch at Galveston, Galveston, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 South Central American Urological Association (AUA) Annual Meeting, Colorado Springs, CO, Wed, Oct 30 – Sat, Nov 2, 2024.
Video Related Content: BRAVO Trial Highlights Improved Detection Reduces Bladder Cancer Recurrence - Ali Nasrallah


