(UroToday.com) The 2024 South Central AUA annual meeting included the resident essay podium presentation competition, featuring a presentation by Dr. Carlos Gonzalez-Martinez discussing whether we can predict locally advanced disease features with PSMA PET by correlating molecular imaging TNM with pathological TNM in radical prostatectomy specimens. PSMA PET with any available agent is one of the most useful and innovative staging methods for prostate cancer.
Currently, the role of the molecular imaging T staging is controversial, as its pathological correlation has not been elucidated. The objective of this study presented at the 2024 South Central AUA annual meeting was to assess the correlation of molecular imaging TNM with pathological TNM.
This was a retrospective study in which patients were included if they were older than 18 years of age with non-metastatic prostate cancer in a referral center in Mexico from 2017-2024, underwent 18F-PSMA-11 PET, and subsequently a radical prostatectomy within less than 12 weeks. Dr. Carlos Gonzalez-Martinez and colleagues performed a Spearman’s Rho analysis for the correlation between locally advanced disease features (seminal vesicle invasion, extraprostatic extension, high risk pathology) in the PSMA PET and their presence in the pathology specimen.
There were 28 patients included with a mean age of 67.4 ± 6.6 years, with a mean PSA at diagnosis of 13.8 ± 8.0 ng/mL, and a mean PSA density of 0.11 ± 1.64. The mean SUVmax on PSMA PET/CT was 11.64 ± 8.38. A summary of the clinical, PSMA PET/CT, and prostatectomy variables is as follows: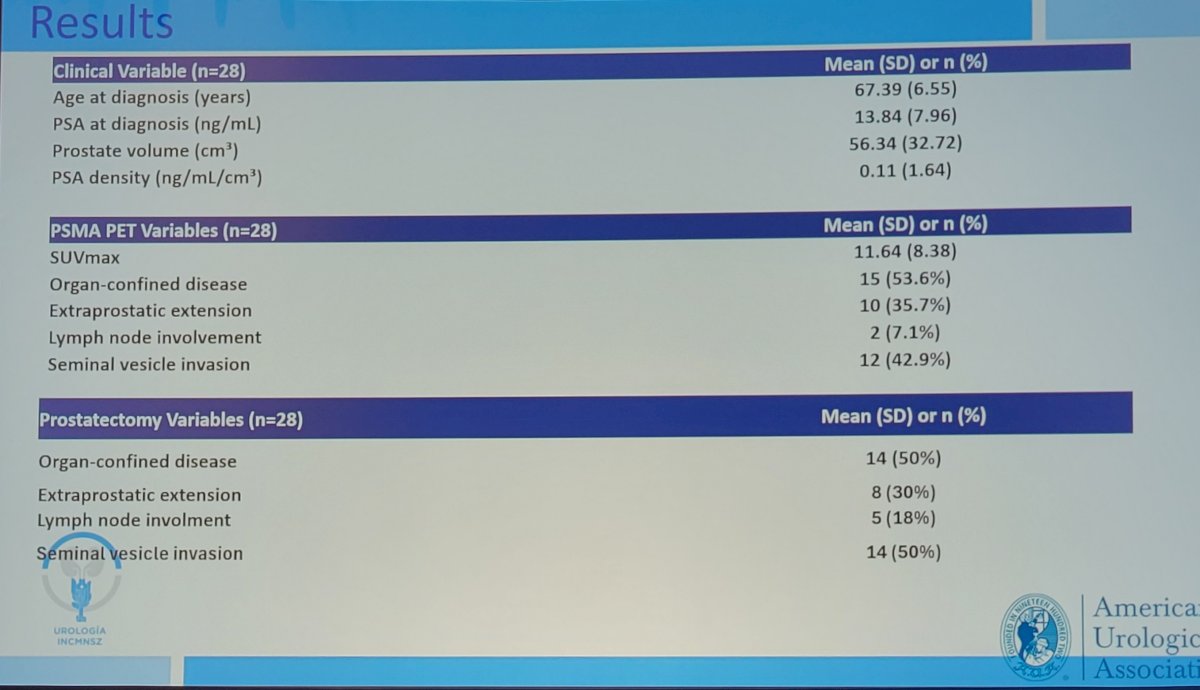
The key finding was a correlation between locally advanced disease in PSMA PET versus locally advanced in the radical prostatectomy pathology specimen with correlation of 0.831 (p< 0.001):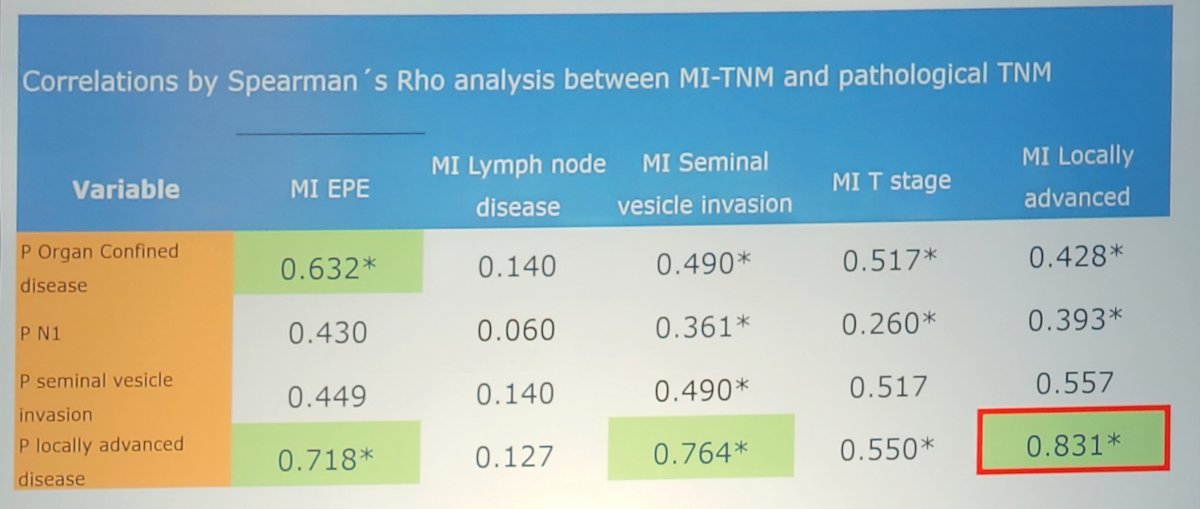
A chi square analysis identified an RR of 20.11 (p <0.001), with and PPV of 100%, NPV of 88.9%, for the risk of locally advanced disease features in the prostatectomy specimen if the PSMA PET showed any adverse feature: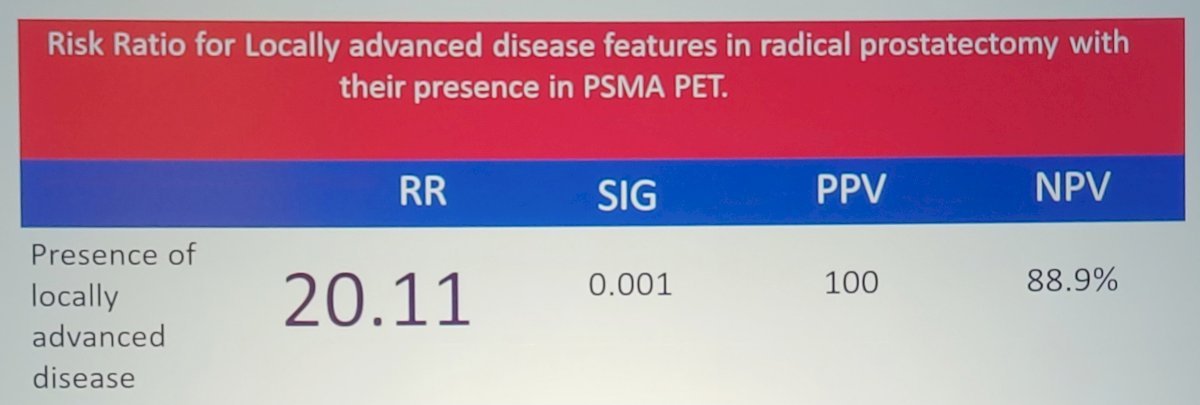
Dr. Gonzalez-Martinez noted several limitations of this study, including:
- A small sample size and a single center experience
- This is the first such study in Mexico and may not be fully representative of other populations
Dr. Gonzalez-Martinez concluded his presentation discussing whether we can predict locally advanced disease features with PSMA PET by correlating molecular imaging-TNM with pathological TNM in radical prostatectomy specimens with the following take-home points:
- This study demonstrates that 18F-PSMA PET findings have a good degree of correlation with pathologic radical prostatectomy specimen and can predict adverse pathologic features such as extraprostatic disease, seminal vesicle invasion, and high grade ISUP
- These results may influence the surgical decision making process, such as inclusion in a multimodal treatment scheme, or a shift from surgery to external beam radiotherapy.
Presented by: Carlos A. Gonzalez-Martinez, MD, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 South Central American Urological Association (AUA) Annual Meeting, Colorado Springs, CO, Wed, Oct 30 – Sat, Nov 2, 2024.


