(UroToday.com) The 2024 South Central AUA annual meeting included a session on lower genitourinary tract cancer, featuring a presentation by Anish Patel discussing 90-day urologic complications from pelvic exenteration at a single, tertiary-level medical center. The management of locally advanced and/or recurrent pelvic malignancies has evolved significantly over the years with improvements in neoadjuvant treatments and perioperative patient care.
Yet, despite these advancements, the practice of performing pelvic exenteration still remains controversial with a high morbidity and surgical complication rates. In this series, the investigators sought to summarize outcomes in a contemporary series with a focus on the urologic outcomes and to investigate which factors were associated with morbidity and survival.
This was a retrospective review of patients who underwent pelvic exenteration at a single tertiary-level medical center from 2009 to 2022 who had a urinary diversion for an underlying malignancy. Patient demographics, comorbidities, neoadjuvant therapy, urinary diversion type (ileal/colonic), and surgical data were recorded. The primary endpoints included 90-day post-operative complication rates, hospital length of stay, ICU course, and survival rates.
There were 39 patients that met inclusion criteria, of which 43.6% were Hispanic. Of the primary malignancies recorded, 38% (n = 15) were urologic, 10% (n = 4) gynecologic, 33% (n = 13) colorectal, and 5.1% (n = 2) soft tissue origin. The mean patient age was 62.8 +/- 12.1 years. Overall, 23.1% (n = 9) of patients had a history of diabetes and 51.3% (n = 20) underwent prior radiotherapy: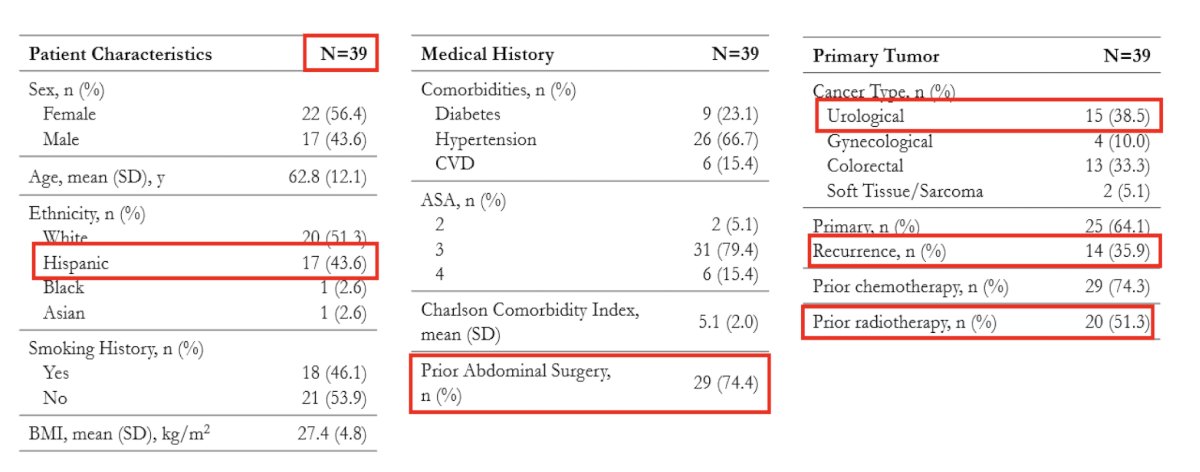
Surgically, 74.4% of patients (n = 29) underwent curative intent, 7 (17.9%) had colonic/sigmoid urinary diversion, while 82.1% (n = 32) had ileal urinary diversion. There were 28.2% (n = 11) of patients that required a ventral rectus abdominus flap (VRAM) or gracilis flap, of which 3 were men. The mean length of stay was 18.9 +/- 21 days. During follow-up, 38% (n = 15) experienced a major complication (Clavien-Dindo 3+), and 6 (15%) patients had a major cardiopulmonary/cerebrovascular event. Overall, 20 patients died (51%), with 26% (n = 10) dying within 1 year of surgery. The readmission rate within 90 days of surgery was 43.6%. Three patients required laparotomy within 30 days, two patients had Clostridium difficile from long use of prophylactic antibiotics, 28% (n = 11) had urine leaks requiring either a nephrostomy tube placement or drain insertion, and 10% of patients (n = 4) had UTIs in the immediate post-operative period: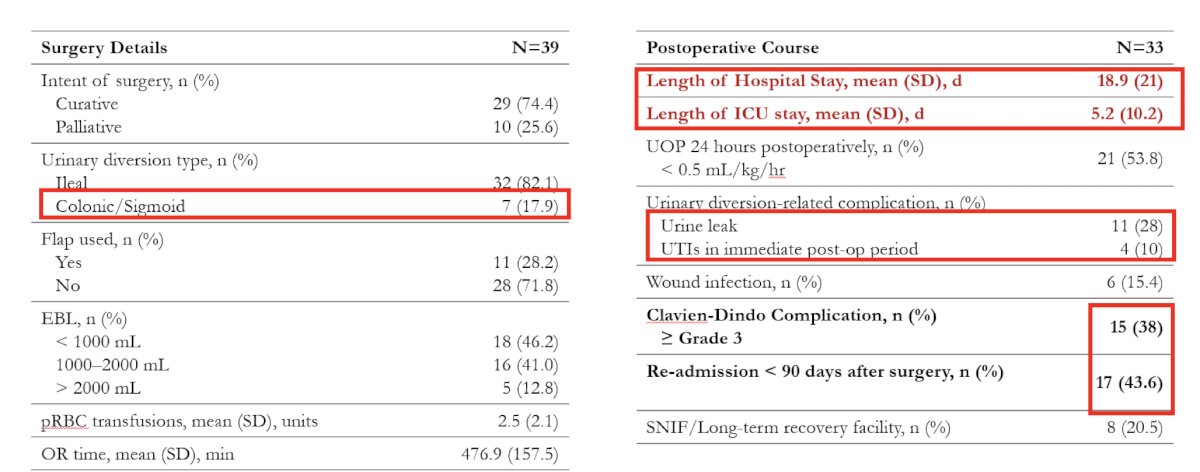
Multivariate regression analysis demonstrated that a history of diabetes was associated with higher Clavien-Dindo complication scores (Coef: 6.367, p < 0.05). History of neoadjuvant chemotherapy trended toward higher Clavien-Dindo scores but was not statistically significant (Coef: 5.75, p = 0.063). Hospital length of stay statistically correlated with BMI (Coef: 1.61, p = 0.046).
Anish Patel concluded his presentation discussing 90-day urologic complications from pelvic exenteration at a single, tertiary-level medical center with the following take-home points:
- Pelvic exenteration is a highly morbid operation that requires a multidisciplinary approach and the resources of a large tertiary medical center
- Patients typically present with late-stage disease and with other medical comorbidities, greatly impacting the surgical complication rates and patient survival.
- There has been an increasing use of sigmoid or more distal colonic conduits instead of ileal conduits, which leads to better outcomes in certain patients (ie. when a VRAM flap is needed)
- Multi-institutional studies are needed to conduct robust statistical analysis of acceptable power.
- Future studies may compare ileal and colonic conduits head to head to determine differences in outcomes.
Presented by: Anish Patel, DO, UT Health San Antonio, San Antonio, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 South Central American Urological Association (AUA) Annual Meeting, Colorado Springs, CO, Wed, Oct 30 – Sat, Nov 2, 2024.


