(UroToday.com) The 2024 South Central AUA annual meeting included an endourology session, featuring a presentation by Dr. Jeffrey Cadeddu discussing multiparametric MRI in the evaluation of small renal masses. Secondary to cross-sectional imaging, there has been a significant increase in the incidental identification of small renal masses.
Notably, the pathology of these masses is unknown as CT is inadequate in confidently differentiating histology. Many of these masses will remain indolent with no/slow growth, in addition to 30% of T1a masses being benign. Moreover, some of these patients will be candidates for active surveillance of their small renal masses.
Based on our guidelines, treatment recommendations do not distinguish based on histology, with the assumption that outcomes of all renal mass subtypes are the same, which is incorrect. Under the section of Evaluation/Diagnosis, the AUA guidelines state:
- Obtain high-quality, multiphase cross-sectional abdominal imaging to optimally characterize the renal mass
- Obtain a CBC, CMP, and US. If malignancy is suspected, metastatic evaluation should include chest imaging and careful review of abdominal imaging.
- Assign CKD stage based on GFR and degree of proteinuria.
Since pathologic subtypes affect outcomes, should all patients have a biopsy prior to treatment recommendation (surgery, ablation, active surveillance)? Historically, renal mass biopsy was not advised given its inaccuracy and risk of tumor seeding. However, now renal mass biopsy is an accepted means of tumor evaluation. The pros of a renal mass biopsy are that it is a definitive diagnosis, thus reducing the number of benign nephrectomies (5% vs 16%).1 The sensitivity is 97.5%, specificity is 97.26%, and PPV is 99.8%. However, the cons of a renal mass biopsy are as follows:
- Invasive:
- Patients do not like it, there is a 1% risk of hemorrhage, associated pain, and hematuria
- Not all tumors are amenable (hilar, anterior)
- 1% increased likelihood of upstaging from cT1a to pT3a (perirenal fat) in RCC
- Risk of tumor seeding is not zero
- Diagnostic performance (meta-analysis):2
- Non diagnostic in 14%
- NPV 63%: 37% of those with a benign biopsy have malignant disease
One alternative to renal mass biopsy for characterizing these tumors is multiparametric MRI (mpMRI). The mpMRI renal protocol includes: T2 weighted, T1 weighted chemical shift imaging, and T1-weighted fat-suppressed dynamic contrast enhancement. The following algorithm is a high-level overview of how a radiologist can interpret a renal mass on mpMRI: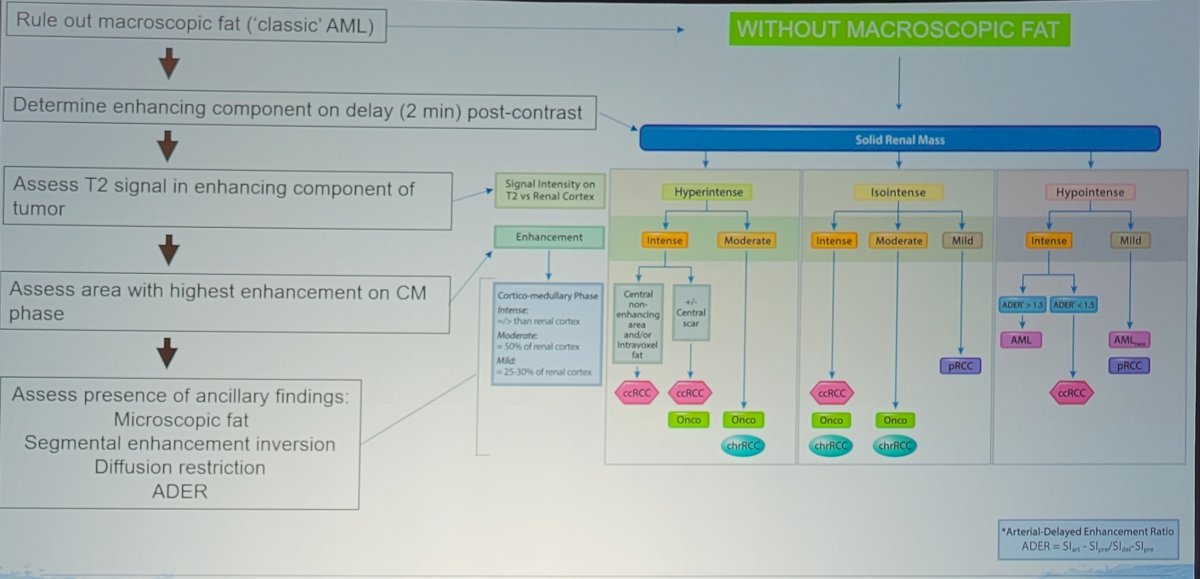
Dr. Cadeddu emphasized that the middle column of the algorithm (Isointense) is where the clinical conundrum occurs, as this could be anything and where renal mass biopsy may play a role.
Since mpMRI appears to be a reasonable means to identify clear cell RCC, a Likert scale was proposed to assess the subjective likelihood of identifying clear cell RCC using mpMRI. This became known as the clear cell Likelihood Score (ccLS), with early work performed by Dr. Cadeddu and his team. The early ccLS was as follows:
- ccLS 1: definitely not clear cell RCC
- ccLS 2: probably not clear cell RCC
- ccLS 3: equivocal
- ccLS 4: probably clear cell RCC
- ccLS 5: definitely clear cell RCC
This has been incorporated into the aforementioned algorithm: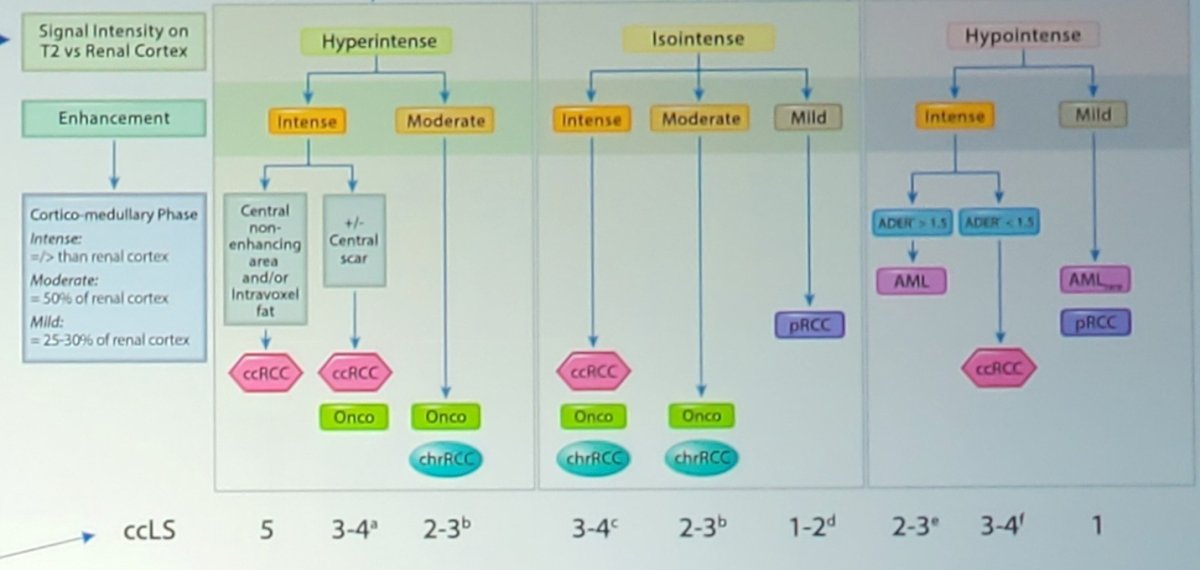
Dr. Cadeddu’s group’s first paper on ccLS was published in 2017, assessing 110 patients with 121 renal masses. Seven radiologists with different levels of experience who were blinded to final pathology findings independently reviewed studies based on a predefined algorithm. Mean tumor size was 2.4 cm and 50% of the lesions were clear cell. Defining clear cell as scores of 4 or greater demonstrated 78% sensitivity and 80% specificity while scores of 3 or greater showed 95% sensitivity and 58% specificity. Interobserver agreement was moderate to good with a mean κ of 0.53. The AUCs ranged from 0.82-0.92 for defining clear cell RCC and ccLS 4-5: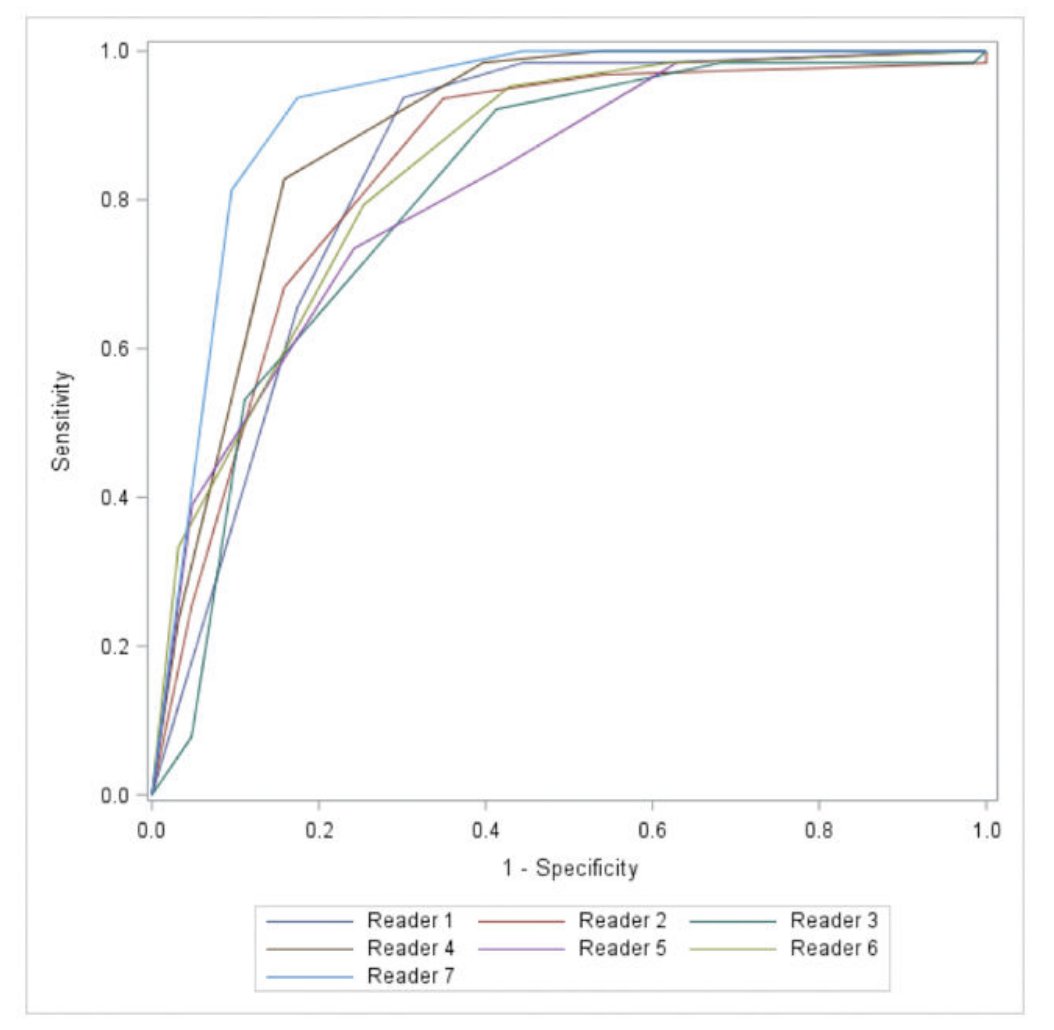
Notably, a ccLS of 1-2 had a PPV of 93% for non clear cell RCC: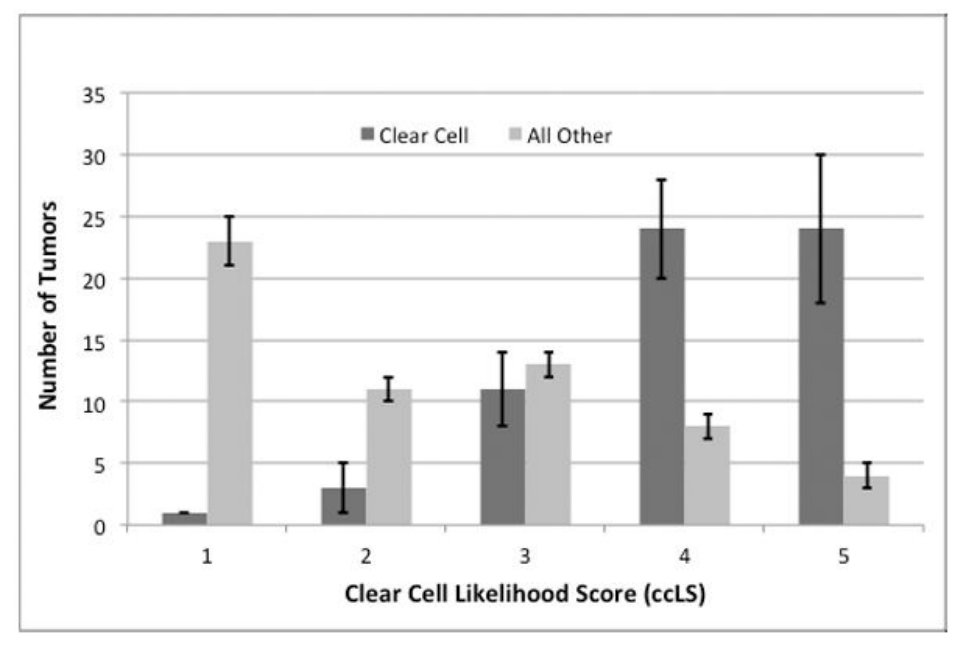
In 2021, Dr. Cadeddu’s group published a validation bi-institutional assessment of ccLS.4 This study included 434 patients with 454 renal masses from two institutions with heterogeneous patient populations that underwent mpMRI with prospective ccLS assignment and had pathologic diagnosis. They found that 94% of ccLS 4-5 tumors are malignant (clear cell, chromophobe, or papillary RCC) and only 5% of ccLS 1-2 harbored clear cell RCC:
Subsequently, in 2022, they further validated ccLS with a multi-institutional cohort of 241 patients at 5 academic institutions.5 After a 1.5-hour training session, two abdominal radiologists per center independently rendered a ccLS for 50 masses. The sensitivity, specificity, and positive predictive value for the diagnosis of clear cell RCC when ccLS was 4 or higher were 75% (95% CI: 68, 81), 78% (95% CI: 72, 84), and 76% (95% CI: 69, 81), respectively. The negative predictive value of a ccLS of 2 or lower was 88% (95% CI: 81, 93). The following shows the ROC curves shows the diagnostic performance of mpMRI ccLS across 10 radiologists: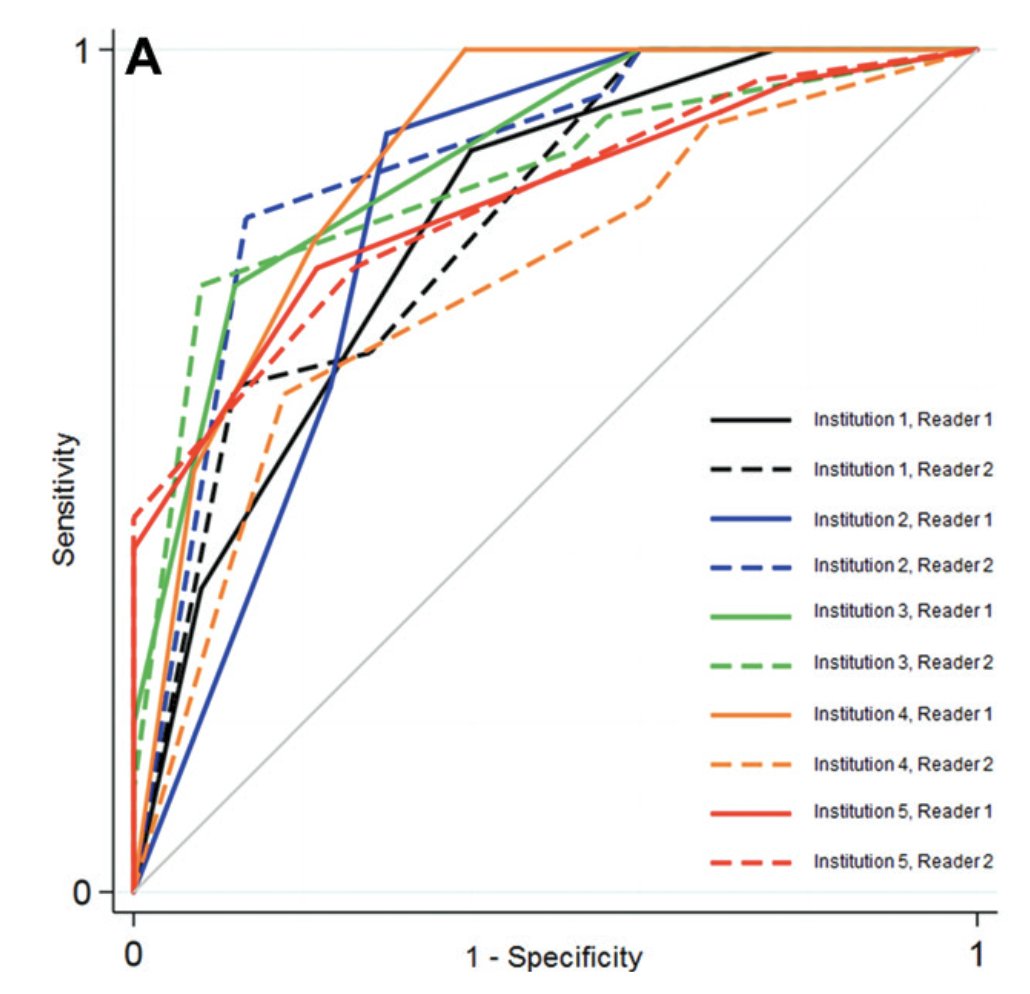
Dr. Cadeddu’s group has also shown the association of ccLS on MRI and growth kinetics of small renal masses on active surveillance.6 In this study, growth rates of 386 SRMs (100 ccLS 1–2, 75 ccLS 3, and 211 ccLS 4–5) from 339 patients (median age, 65 years; 198 men, 141 women) were analyzed. The ccLS was correlated with growth rates by size (ρ = 0.19; p < 0.001; ccLS 4–5, 9%/year; ccLS 1–2, 5%/year; p < 0.001):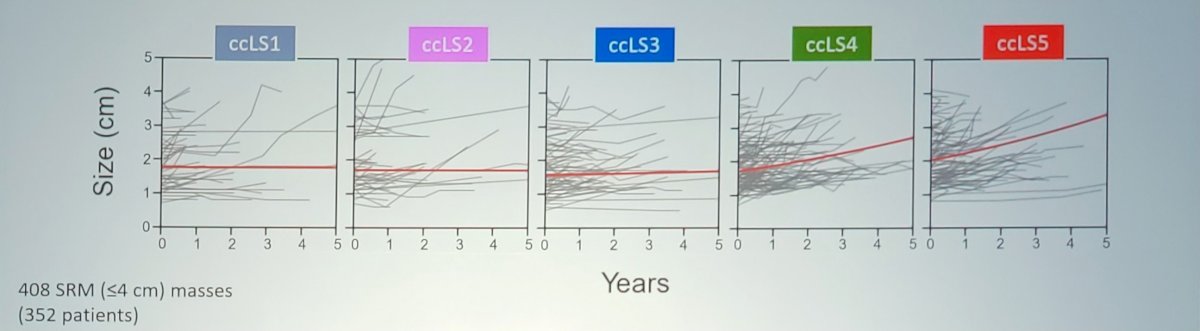
This was also associated with volume (ρ = 0.14; p = 0.006; ccLS 4–5, 29%/year; ccLS 1–2, 16%/year; p < 0.001).
The group at the University of Virginia recently performed a cost-effectiveness analysis of the ccLS against renal mass biopsy for small renal masses.7 They found that the ccLS was both more effective (0.77 vs 0.70) and less expensive than renal mass biopsy ($1629 vs $1966). Sensitivity analysis found that the non-diagnostic rate of renal mass biopsy and the sensitivity of the ccLS had the greatest impact on the model. In threshold analyses, the ccLS was the preferred strategy when its sensitivity was greater than 62.7% and when an MRI cost less than $5332.
Dr. Cadeddu’s algorithm that he uses in his practice for cT1a renal masses is as follows:
- ccLS 4 and 5: consider intervention without biopsy
- Clear cell RCC PPV: 89%
- 95% of ccLS 5 tumors are malignant (RCC any type)
- ~90% of ccLS 4 tumors are malignant (RCC any type)
- ccLS 1 and 2: encourage active surveillance if appropriate (particularly for cT1a <3 cm)
- Clear cell RCC NPV is 96% for cT1a tumors
- >85% are papillary and chromophobe RCC
How may ccLS assist with management? If we only consider ccLS 3 tumors for a possible biopsy, this constitutes 20% of all T1a tumors. Overall 40% of these will be clear cell RCC, 20% will be papillary or chromophobe RCC, and 40% will be benign and indolent. Thus, biopsy has the highest diagnostic yield for ccLS 3 tumors, meaning if we biopsies all ccLS 3 tumors we would only be biopsying 20% of all small renal masses.
Dr. Cadeddu concluded his presentation discussing multiparametric MRI in the evaluation of small renal masses with the following take-home points:
- mpMRI is a promising means of renal tumor characterization versus biopsy
- ccLS:
- Can reliably identify most clear cell RCCs
- Assists in decision-making for cT1a tumors
- Eliminates biopsy for most tumors
- Is cost-effective
Presented by: Jeffrey Cadeddu, MD, UT Southwestern University, Dallas, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 South Central American Urological Association (AUA) Annual Meeting, Colorado Springs, CO, Wed, Oct 30 – Sat, Nov 2, 2024.
References:
- Richard PO, Lavallee LT, Pouliot F, et al. Is Routing Renal Tumor Biopsy Associated with Lower Rates of Benign Histology following Nephrectomy for Small Renal Masses? J Urol. 2018 Oct;200(4):731-736.
- Patel HD, Johnson MH, Pierorazio PM, et al. Diagnostic accuracy and risks of biopsy in the diagnosis of a renal mass suspicious for localized renal cell carcinoma: Systematic review of the literature. J Urol. 2016 May;195(5):1340-1347.
- Canvasser NE, Kay FU, Xi Y, et al. Diagnostic accuracy of multiparametric magnetic resonance imaging to identify clear cell renal cell carcinoma in cT1a renal masses. J Urol. 2017 Oct;198(4):780-786.
- Steinberg RL, Rasmussen RG, Johnson BA, et al. Prospective performance of Clear Cell Likelihood Scores (ccLS) in Renal Masses Evaluated with Multiparametric Magnetic Resonance Imaging. Eur Radiol. 2021 Jan;31(1):314-324.
- Schieda N, Davenport MS, Silverman SG, et al. Multicenter Evaluation of Multiparametric MRI Clear Cell Likelihood Scores in Solid Indeterminate Small Renal Masses. Radiology. 2022;303:590-599.
- Rasmussen RG, Xi Y, Sibley III RC, et al. Association of clear cell likelihood score on MRI and growth kinetics of small solid renal masses on active surveillance. AJR. 2022;218:101-111.
- Chen KY, Lange MJ, Qiu JX, et al. Cost-effectiveness analysis of the Clear Cell Likelihood Score against Renal Mass Biopsy for Evaluating Small Renal Masses. Urology. 2024;188:111-117.


