(UroToday.com) The first panel on the Urologic Workforce Shortage at the American Urological Association’s Advocacy Summit featured leaders in AUA census data, workforce research, and patient advocacy champions. Dr. Andrew Harris, chair of the AUA Workforce Task Force from the University of Kentucky, moderated the session.
To start the conversation, Dr. Amanda North outlined how physicians can leverage AUA census data to understand the urologic workforce shortage. The supply shortage of urologists results from inadequate numbers of Graduate Medical Education funding, limiting the number of trainees who enter the specialty. Although the number of medical school graduates has increased, residency slots have not had a proportional increase in growth. There are still urology consistently “unmatched” rates over 20%. Further, the workforce is aging – nearly 30% of urologists are over the age of 65 years old, and 50% are over 55 years. Dr. North highlighted that this disproportionately impacts rural urologists, who tend to be older and approaching the age of retirement. Younger urologists tend to practice in more urban areas, which exacerbates the rural urologist shortage. 90% of urologists practice in a metropolitan area.
Next, Dr. North outlined considerations specific to the female workforce in urology. Female physicians tend to work in academic settings, work in urban areas, spend more time with each individual patient during an encounter leading to fewer patients overall, and plan to retire at an earlier age than men. She emphasized that these factors are important to understand, given that women urologists are entering the field in higher numbers. Trends in insurance status have also changed, as the uninsured rate has reached an all-time low in 2022 after implementation of the Affordable Care Act – this correlates with an increase of patients who seek access to urologic care. Dr. North concluded that this information provides critical context to understand when advocating for workforce issues in urology.
Dr. Christine Van Horn next reviewed changing demographic trends in the urologic workforce. Today, the majority of the workforce is Caucasian, with 4.9% Hispanic, 13.8% Asian, and 2.2% African American urologists currently practicing. From 2014 to 2022, the number of female urologists rose from 7.7% to 11.6%. The trainee demographics vary vastly from this: in 2024, 31% of trainees are female and 45% of women who matched into urology are women. She emphasized that racial/ethnic diversity is also rapidly rising within the trainee workforce. Attrition rates within both residency and post-training practice are important to understand. Both racial/ethnic minority trainees and women practicing urologists show disproportionately higher attrition rates. Almost 40% of women in medicine transition to part-time work within their first 6 years of practice – Dr. Van Horn concluded by emphasizing that we must understand the root of these problems to reduce the number of urologists leaving the workforce.
Following Dr. Van Horn, Dr. Kathleen Kieran presented her perspective on recruiting urologists to practice in rural settings. Based on a survey study she conducted, urologists who choose to work in rural areas cited job satisfaction, increased control over clinical practice, and proximity to family as reasons for geographic practice settings. Further, she outlined that 49% grew up in a non-metropolitan (NMP) setting, 52% were exposed to NMP healthcare in medical school, but less than 25% were exposed to rural care in residency. This survey also found that resource strain, call burden, and care coordination are stressors for rural urologists. Dr. Kieran emphasized these areas as being potential areas for focused improvement to retain and recruit urologists to rural areas. Rural hospitals are closing at high rates due to limited financial resources, low staffing numbers of nursing and ancillary staff, and other resource strains. In addition, the call burden for rural urologists is significantly higher than in a metropolitan practice. Survey respondents reported that 46% take calls more than 10 days per month, and cited this single issue as the reason they plan to retire early. In conclusion, Dr. Kieran presented potential solutions to improve the rural workforce shortage. She encouraged community and collaboration between rural communities and tertiary/quaternary referral centers, as well as creative resource provisions that address limited imaging, pharmacy, and specialty procedure access.
Lastly, Liz Leff, the AUA’s Patient Advocacy Liaison shared the patient's perspective on the ongoing urologic workforce strain. Leff emphasized that the patient is the end-user of healthcare, and limited access to specialty care significantly affects outcomes. She cited a reduction in patient satisfaction and used data from COVID-19 related care disruptions to quantify increased anxiety and reduced quality of life.
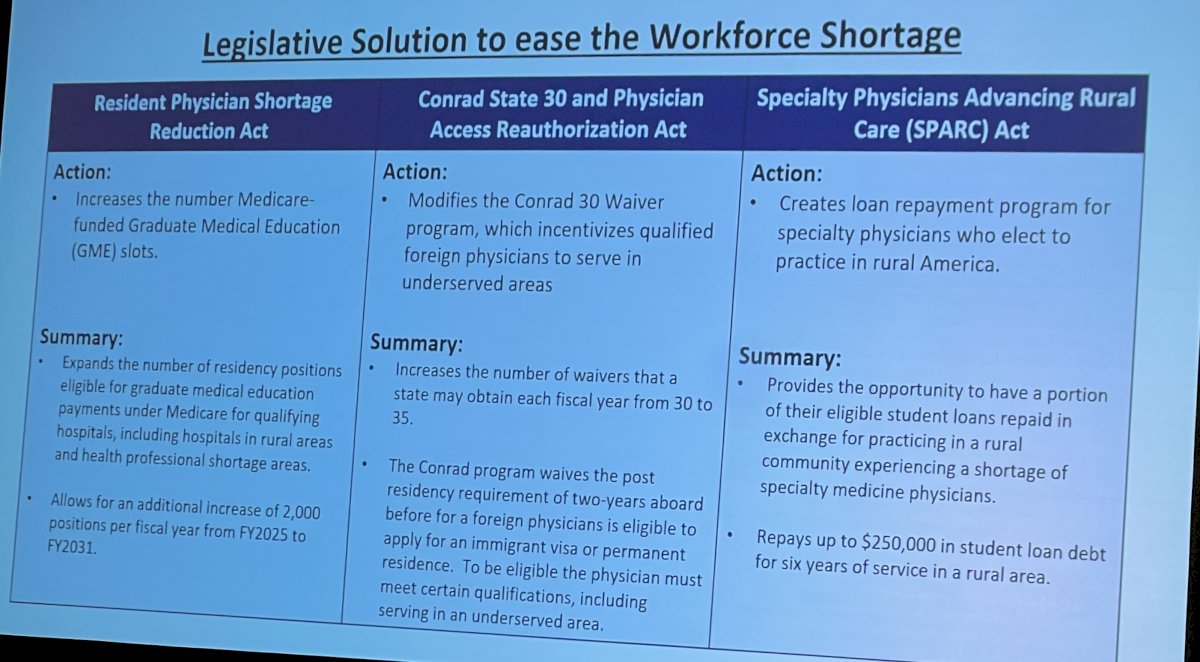
Dr. Harris concluded the panel by highlighting legislative solutions to ease the workforce shortage, outlined below:
- Christine Van Horn, MD, Member, Society of Women in Urology
- Amanda North, MD, Chair, AUA Data Committee; Member, Societies for Pediatric Urology
- Kathleen Kieran, MD, Western Section; Liz Leff, AUA Patient Advocacy Liaison
- Andrew Harris, MD, Moderator, Chair, AUA Workforce Task Force


