(UroToday.com) The American Urological Association’s 2024 Advocacy Summit included a session on Medicare Payment Reform. Dr. Jonathan Rubenstein began this session by outlining the history and current state of physician payment. In 1965, President Johnson signed Medicare into law. Over the years, payment policy has evolved, but it remains budget neutral. He emphasized the fact that physician payment is the only aspect of Medicare that is not tied to inflation.
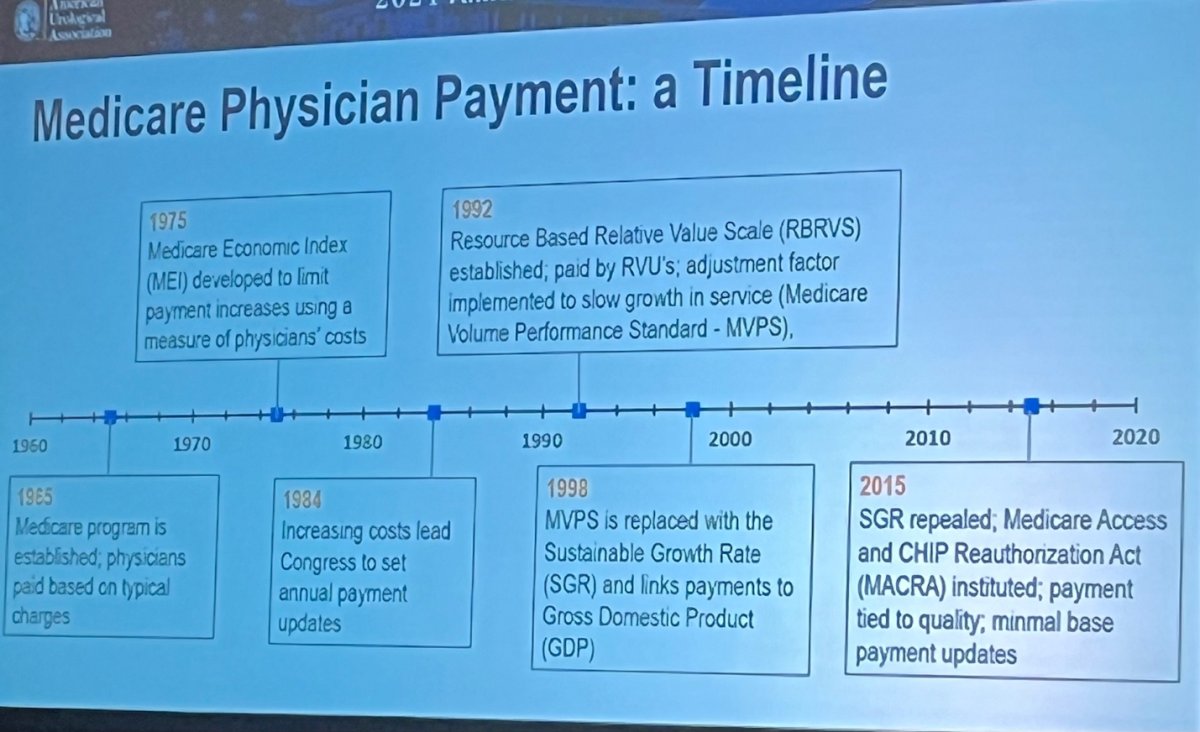
In 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) was instituted, which instituted quality based payment incentives but did not have any base payment updates. In addition to the lack of inflation adjusted reimbursement, in 2024, all aspects of Medicare related healthcare reimbursement increased, except for physician payments. In response, Dr. Rubinstein stated that independent physicians cannot maintain individual practices. Physician groups have continued to consolidate due to downward financial pressure, selling practiceto health system and private equity. Practices that service the Medicare population are especially affected by this.
Erika Miller, JD, provided insight into the limited Congressional actions concerning physician payments, specifically addressing the stagnation of physician payment due to the unchanged “conversion factor” over the past two decades. She encouraged those at the Summit to advocate for two key actions from Congress: an immediate resolution for the 2024 conversion factor within this year's fee schedule, and comprehensive structural changes to the Medicare Physician Payment system to prevent ongoing annual reimbursement concerns. Miller highlighted that meaningful reform would involve updating the conversion factor with inflation through the Medicare Economic Index, revising budget neutrality rules, updating practice expense inputs periodically, and overhauling the Quality Payment Program (QPP) to ease administrative burdens and foster meaningful engagement by medical practices. The bipartisan House bill, H.R. 2474, known as the Strengthening Medicare for Patients and Providers Act, has been proposed to implement these significant reforms, including an inflationary adjustment for the conversion factor.
Dr. Joshua Langston provided the Large Urology Group Practice Association (LUGPA) viewpoint on the topic of physician compensation reductions. He articulated that the Medicare Physician Fee Schedule impacts urology practices across the board, including community-based, academic institutions, large groups, and solo practitioners. Dr. Langston clarified that the goal of physicians is not to seek higher wages but rather to maintain consistent compensation that supports the delivery of high-quality medical care and promotes the growth and stability of the workforce to meet the needs of the population. He pointed out that the trend towards consolidation in the healthcare industry poses a threat to patient access, as it tends to concentrate services in urban centers and drive-up overall healthcare expenses. Dr. Langston concluded by reinforcing the need for physicians to remain engaged in advocacy with Congress, to match the political efforts of pharmaceutical companies and hospital organizations, and to ensure the continued provision of high-quality, valuable care for the American populace.
Presented by: Jonathan Rubenstein, MD, AUA Current Procedural Terminology (CPT) Advisor; Erika Miller, JD, CRD Associates; Joshua Langston, MD, LUGPA Health Policy Committee
Written by: Ruchika Talwar, MD, Urologic Oncology Fellow, Vanderbilt University Medical Center, during the 2024 AUA Advocacy Summit, Feb 26 to Feb 28, 2024


