One of the most important advances in testis cancer research is the utilization of miRNA based on its prognostic and predictive value. The two most common miRNAs in testicular germ cell tumors include miR-371-373 and miR-302, which are present in seminoma and non-seminoma, and both adult and pediatric patients.
Several early studies in this field have shown that miRNAs are more sensitive and specific than existing tumor makers. miRNA is detectable in the serum whereby they are released into the bloodstream via exosomes and are resistant to degradation. Furthermore, they have a short half-life (T1/2 of 3-7 hours), compared to beta-HCG (36 hours) and AFP (5-7 days). First presented at the 2019 American Society of Clinical Oncology - Genitourinary Symposium (ASCO GU 2019) by Dr. Hamilton, as follows is a table describing the varied methods of assessing miRNA:

A study published in 2019 by Nappi et al.1 assessed specificity and positive predictive value by mapping plasma miR371 expression to actual clinical events in patients with a history of germ cell tumors. Among 111 patients, 46 (35%) of 132 samples had clinically confirmed active germ cell malignancy over the course of management; among these patients, 96% had plasma miR371 expression (true positives) with no false positives. Furthermore, plasma miR371 expression in confirmed active germ cell malignancy had a specificity, sensitivity, positive predictive value, and negative predictive value of 100%, 96%, 100%, and 98%, respectively. Recent work from Dr. Hamilton’s group assessed the ability of serum miRNAs to predict residual viable nonseminomatous germ cell tumors after chemotherapy.2 They found that miRNA levels were significantly associated with disease extent at chemotherapy and they decreased significantly after chemotherapy. Additionally, miR-371a-3p demonstrated the highest discriminative capacity for viable germ cell tumors (area under the curve [AUC] 0.874 95% confidence interval [CI] 0.774-0.974, p <0.0001).
An important ongoing prospective study that will continue to clarify the role of miRNA in testis cancer is the SWOG S1823 trial “Prospective cohort study of miR-371a-3p for tumor surveillance in stage I testicular cancer”: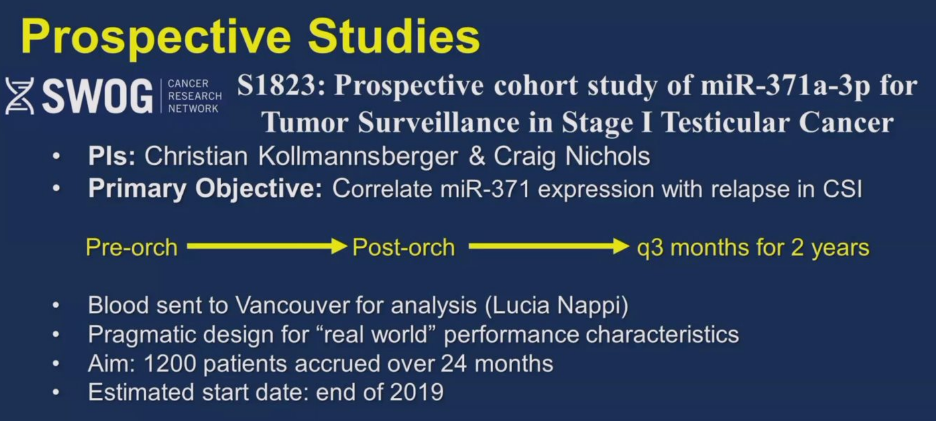
Additionally, the Children’s Oncology Group has the ongoing AGCT1531 study “Minimizing toxicity for low and standard risk pediatric, adolescent and young adult germ cell tumor patients” and ANZUP has the CLIMATE trial “Assessing the clinical utility of miR-371 as a marker of residual disease in clinical stage 1 testicular germ cell tumor, following orchiectomy”. Both of these trials are parallel studies to the SWOG S1823 study with an agreement to combine data for larger analysis. Dr. Hamilton notes that there is important retrospective data to date, but it will be exciting and important to see the outcomes of these prospective studies.
With regards to the role of primary retroperitoneal lymph node dissection (RPLND), Dr. Hamilton notes that for patients with stage IIA non-seminomatous germ-cell tumors (NSGCT) (either de novo or progression on surveillance), this is a viable option, particularly if the procedure can be performed robotically with the same oncological principles as the open approach. Additionally, Dr. Hamilton notes that the robotic approach offers the opportunity to perform an excellent nerve-spare and these patients are often discharged on postoperative day 1. Primary RPLND for seminoma is currently being evaluated in several clinical trials including the PRIMETEST and SEMS trials, with data hopefully being reported in the near future. The PRESTIGE study is an ongoing trial with the following trial schema:
Presented by: Robert Hamilton, MD, MPH, FRCSC, Clinician Investigator, Cancer Clinical Research Unit (CCRU), Princess Margaret Cancer Centre, Toronto, Canada
Ben Tran, MBBS, FRACP, Consultant Medical Oncologist, Peter MacCallum Cancer Centre, Clinical Trials Lead, VCCC Uro-Oncology Trials Program, Chair, GU Tumour Group within Cancer Trials Australia (CTA), Deputy Chair, Germ Cell Subcommittee, ANZUP Group, Melbourne, Australia
Fritha Hanning, MB ChB, FRACP, Medical Oncologist, Auckland City Hospital, Chairperson and Initiator, Genitourinary Special Interest Group for New Zealand, New Zealand Representative, ANZUP Group, Auckland, New Zealand
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md during the 2020 Australian and New Zealand Urogenital and Prostate Cancer Trials Group (ANZUP) Mini Annual Scientific Meeting (ASM), November 29 - 30, 2020
References:
1. Nappi, Lucia, Marisa Thi, Amy Lum, David Huntsman, Bernie J. Eigl, Christopher Martin, Brock O’Neil et al. "Developing a highly specific biomarker for germ cell malignancies: plasma miR371 expression across the germ cell malignancy spectrum." Journal of Clinical Oncology 37, no. 33 (2019): 3090.
2. Leão, Ricardo, Ton van Agthoven, Arnaldo Figueiredo, Michael AS Jewett, Kamel Fadaak, Joan Sweet, Ardalan E. Ahmad et al. "Serum miRNA predicts viable disease after chemotherapy in patients with testicular nonseminoma germ cell tumor." The Journal of urology 200, no. 1 (2018): 126-135.


