(UroToday.com) In this session, Dr. Dana Rathkopf discusses germline testing recommendations for men with prostate cancer. Guidelines agree that all men with metastatic prostate cancer should undergo germline testing and recommendations are evolving across the rest of the disease spectrum. New in 2021, the NCCN guidelines recommended germline testing for men with high and very high risk localized prostate cancer and to consider testing for men with intermediate risk and intraductal/cribriform carcinoma.
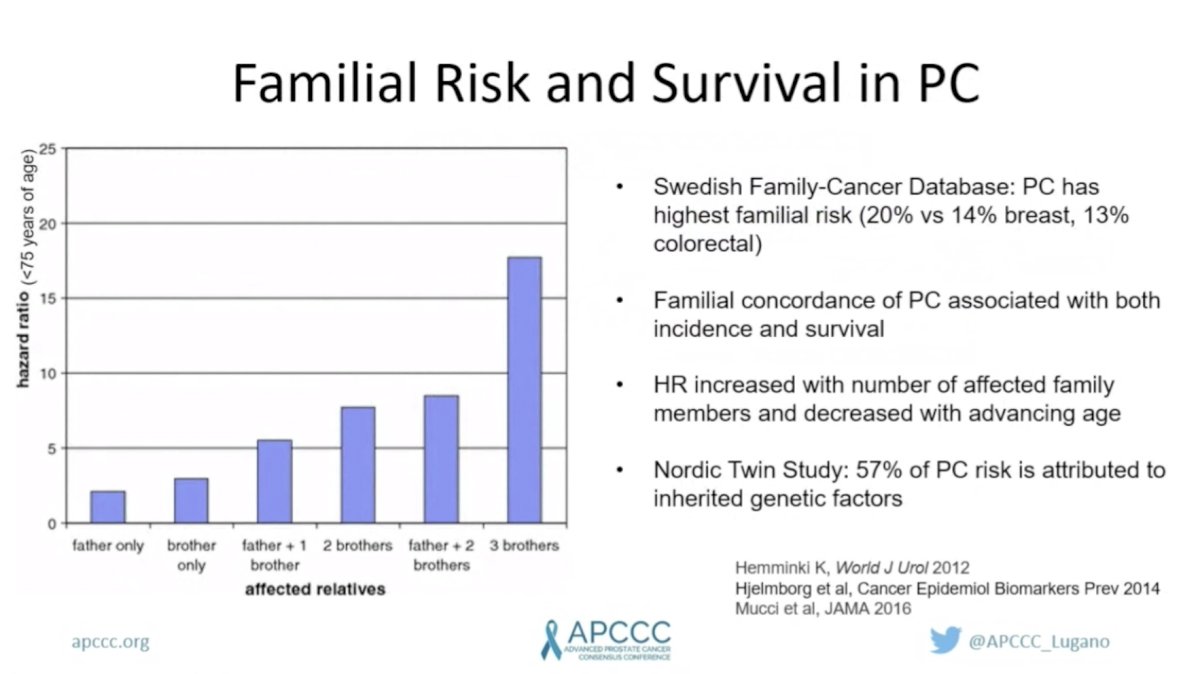
Family history or personal history of cancer factors strongly into recommendations. Men of Ashkenazi ancestry and/or family history of known germline variants are recommended to undergo testing. Family history of ovarian, breast, and pancreatic cancer are associated with BRCA1/2 alterations. Lynch syndrome is associated with colorectal, endometrial, gastric, and upper tract urothelial cancers. Independent of known germline alterations, the risk of prostate cancer increases with the number of affected family members. The Nordic Twin study reported that 57% of prostate cancer risk is attributed to inherited genetic factors. GWAS studies have identified DNA variants that are associated with prostate cancer risk ranging from rare highly penetrant alterations (such as TP53 and BRCA2) to common low penetrant alterations, which are most commonly in non-coding DNA. While each of these variants imparts only a small risk, polygenic risk scores based on common variants have been associated with significant prostate cancer risk.
Integrated germline and somatic analysis of 150 men with mCRPC identified DNA damage repair (DDR) alterations in nearly one in four (23%) men with mCRPC. The majority (13%) were in BRCA2. Approximately 8% of men harbored germline DDR alterations with BRCA2 again being the most common. A subsequent study by Pritchard et al found germline DDR mutations in 12% of men with metastatic prostate cancer. Notably, mutation frequencies did not associate with family or age of prostate cancer onset, leading to the blanket recommendation for testing all men with metastatic prostate cancer.


Having established the prevalence of germline DDR alterations, Dr. Rathkopf described their clinical relevance as it pertains to prostate cancer risk, disease aggressiveness, and response to therapy. Consistent with it being the most common germline DDR alteration in men with metastatic prostate cancer, germline BRCA2 alterations have the strongest association with developing prostate cancer and are most associated with aggressive disease. Fortunately, BRCA2 alterations are also most predictive of response to PARP inhibitors and platinum chemotherapy.

HOXB13 G48E is a rare, but important germline mutation with a strong association with early-onset prostate cancer. A population-based study of this variant found that carriers had a 33% lifetime risk of developing prostate cancer. HOXB13, a transcription factor, is involved in regulating AR target genes involved in prostate cancer development and growth. There is currently no therapeutic intervention targeting this alteration, but it has significant implications for screening.

The 2019 Philadelphia Prostate Cancer Consensus Conference provided recommendations on which genes should be tested in which populations. The strongest recommendations were for broad germline panel testing for men with metastatic disease, they recommended broad germline panel testing and BRCA2 and HOXB13 for unaffected men with a family history of cancer.

Dr. Rathkopf then emphasized an important point about variation in the prevalence of germline alterations across different ancestral groups. She highlighted the relative paucity of data for non-Caucasian groups and stressed the importance of further research to define the scope of germline alterations in diverse populations.

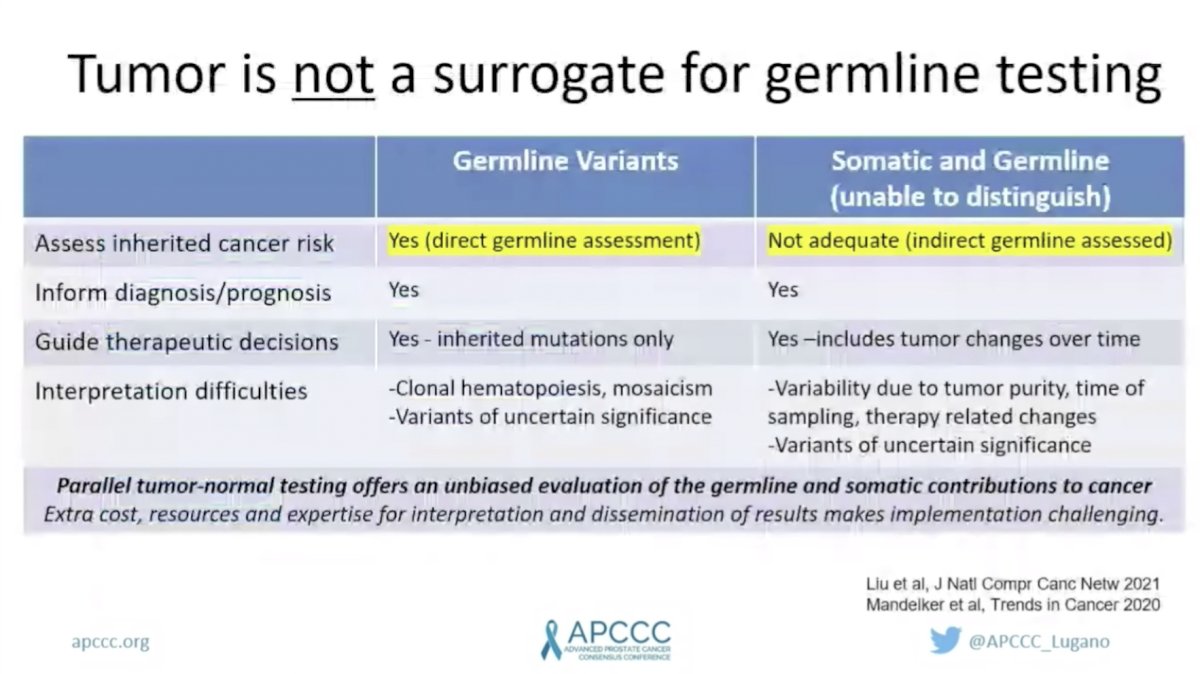
Dr. Rathkopf emphasized that tumor genomic profiling is not a surrogate for germline testing. While it provides important information to inform prognosis and guide therapy decisions, somatic testing does not adequately assess inherited cancer risk. Up to 8% of germline mutations may be missed if only somatic testing is performed.
Finally, Dr. Rathkopf provided a brief overview on interpreting germline results and genetic counseling. There are three broad results that can be returned from germline testing: positive, uncertain, and negative. Post-test counseling is different for each of these scenarios. While clinicians are encouraged to be able to discuss the implications of germline testing results, the gold standard is for patients to meet with a Genetic Counselor. Unfortunately, availability and accessibility to Genetic Counselors is an ongoing limitation. New point of care and electronic education models are being increasingly implemented to overcome this challenge.

Dr. Rathkopf concluded by re-emphasizing that all men with metastatic prostate cancer should undergo germline testing. Other factors including family history, personal history of cancer, and tumor features should be considered in deciding which other patients should be tested. Multiple germline testing options are available and should be selected based on risk management for patient and family and potential impact on prognosis and treatment. For metastatic prostate cancer multi-gene testing is recommended.
Presented by: Dana Rathkopf, MD, Medical Oncologist at Memorial Sloan Kettering Cancer Center
Written by: Jacob Berchuck, MD, Genitourinary Medical Oncologist, Dana-Farber Cancer Institute (Twitter: @jberchuck) during the 2021 Advanced Prostate Cancer Consensus Conference, Saturday, October 9, 2021.


