(UroToday.com) In the session of the 2022 Advanced Prostate Cancer Consensus Conference focusing on the treatment of patients with oligometastatic and oligoprogressive prostate cancer, Dr. Ost examined whether we have predictors for the successful treatment of patients with oligometastatic prostate cancer.
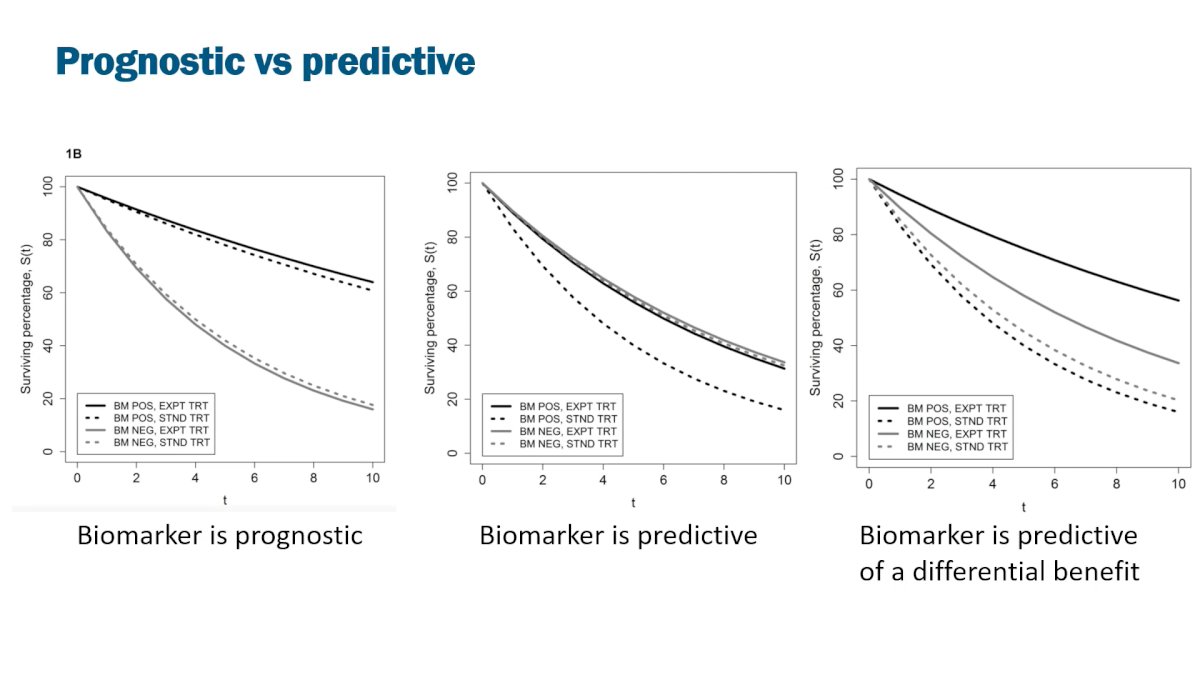
To begin, he noted that interest and enthusiasm for metastasis-directed therapy (MDT) has grown rapidly over the past 10 years. However, this enthusiasm may have grown at a faster rate than the data to justify it. Certainly, today, we need to examine if we have the ability to identify those patients who will actually benefit from MDT. To contextualize this, he first emphasized the importance of distinguishing between biomarkers that are prognostic of outcome (independent of treatment administered) and those that are predictive of response to therapy. Additionally, however, we may consider a biomarker which is predictive of a differential benefit (that is, patients benefit whether biomarker positive or negative but the benefit is greater in one group than the other).
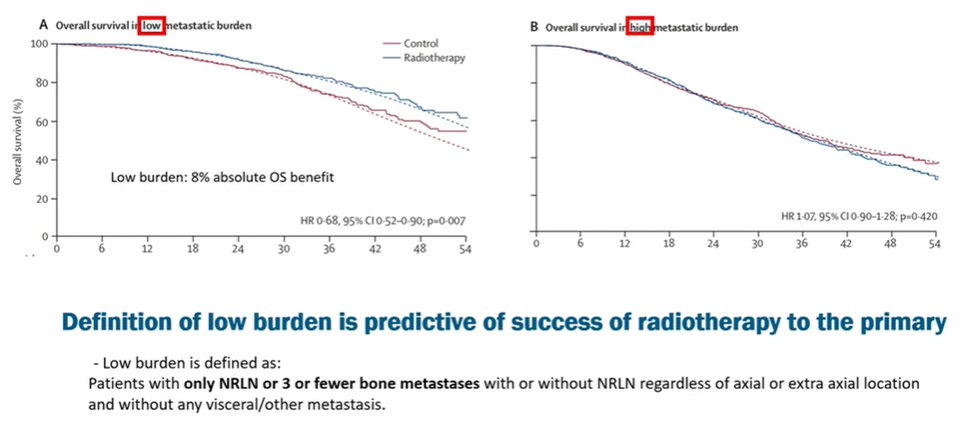
This said, he moved on to examine first data in the context of synchronous metastatic hormone sensitive prostate cancer (mHSPC). Here, he noted that imaging is strongly predictive of outcome. Citing data from the STAMPEDE trial examining local prostate-directed therapy in the context of mHSPC, a relevant (predictive) biomarker is counting of metastatic disease sites: the benefit of local prostate radiotherapy is restricted to patients with a low burden of disease, defined as non-regional lymphadenopathy or three or fewer bone metastases in the absence of visceral metastases.
However, we may potentially move beyond conventional imaging approach. He highlighted work that his own group has done to examine molecular biomarkers in this setting. While prognostic rather than predictive, they identified molecular differences (including PT53, BRCA2, PIK3CA, RB1, and APC) which were differentially noted between patients with high and low burdens of disease. Moving forward, he suggested a biology-guided treatment approach (for example, as is being assessed in the context of the ProBio Trial) may be most appropriate.
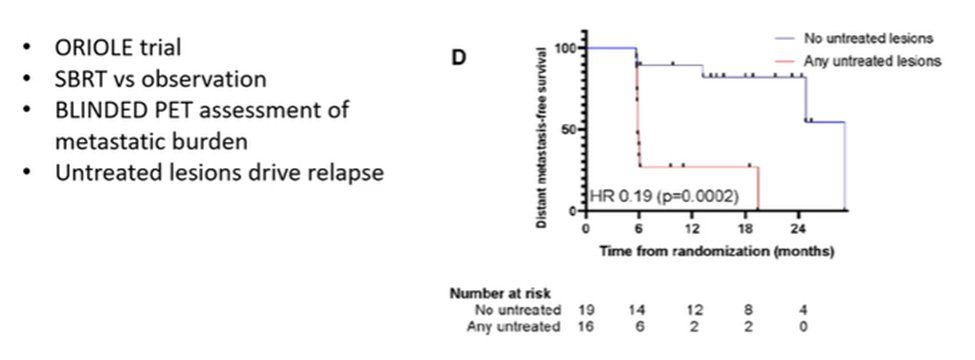
Moving next to a discussion of the metachronous disease space, he again cited the importance of imaging as a predictor. Dr. Ost noted that it has been recognized for 25 years that there is an inability of recognize all metastases, based on the limitations of our imaging approaches. In the past few years, PSMA-PET has gained increasingly large importance in the management of these patients. Based on data from the ORIOLE trial, blinded PET was performed but not used to guide therapy. Among patients where the PET imaging was concordant with conventional imaging (therefore, all sites of disease were treated with MDT) outcomes were significantly better than those where PSMA identified a greater burden of disease (and thus, the discordant disease was untreated).
Again, Dr. Ost considered the potential for molecular data to act as a predictor in this disease space. Again, there are identified molecular differences (including CDK12 and FOXA1) between de novo and recurrent mHSPC. However, there are further differences within each disease state. He emphasized that patients with lung metastases may have a more favourable prognosis and more favourable underlying biology. Assessing this hypothesis of a molecularly defined subset who may not benefit from MDT, he described a combined analysis of the ORIOLE and STOMP trials in which targeted sequencing of the primary tumor or blood was performed to identify patients with high risk mutations. As highlighted in the figure below, overall outcomes were worse among patients with these high-risk mutations. However, there remained a benefit (and even a larger benefit) to the use of MDT in this subset.
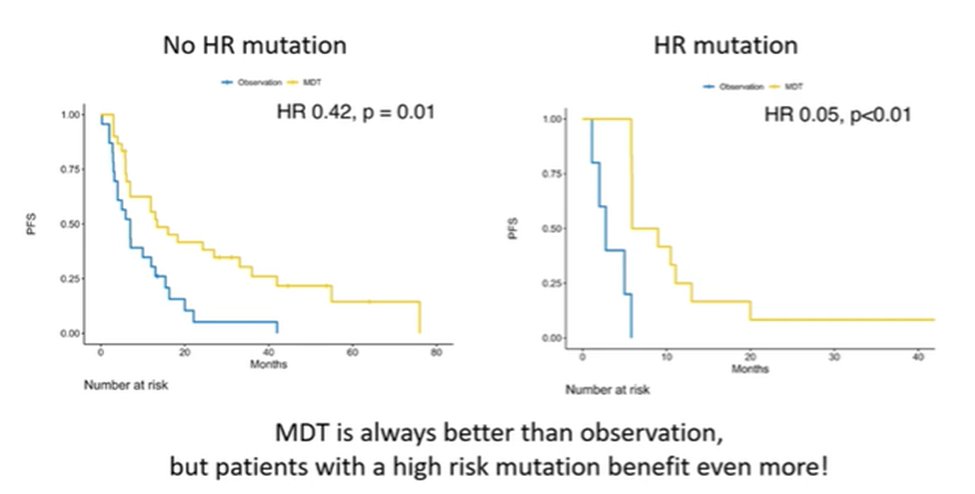
On the basis of this poor prognosis in this subset, Dr. Ost emphasized that systemic therapy treatment intensification is warranted in this subset.
In summarizing, Dr. Ost emphasized that a radiographic definition of disease volume is predictive of the success of primary prostate radiotherapy in de novo mHSPC, though there are no data for MDT. In recurrent disease, he emphasized the importance of using the most sensitive imaging available.
Presented by: Piet Ost, MD, PhD, associate professor at Ghent University, Ghent, Belgium, and radiation oncologist at the Iridium Network, Antwerp, Belgium.


