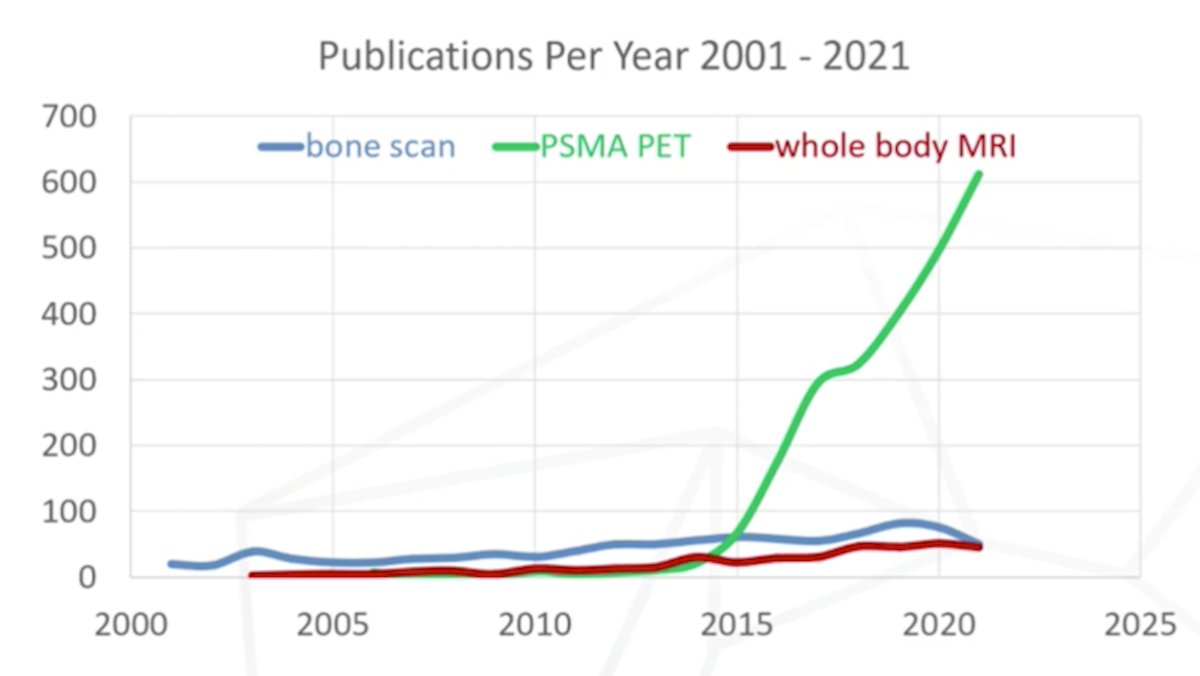
(UroToday.com) The 2022 Advanced Prostate Cancer Consensus Conference (APCCC) Hybrid Meeting included a session on the management of metastatic hormone sensitive prostate cancer (mHSPC) and a presentation by Dr. Michael Hofman discussing how frequent low-volume disease on conventional imaging becomes high-volume on next-generation imaging. Dr. Hofman started his presentation by noting that there has been an explosion of PSMA PET publications per year from 2001 to 2021:
To highlight the low-volume on conventional imaging and high-volume on PSMA PET/CT, Dr. Hofman provided the following example:

Based on data from STAMPEDE ARM H, metastatic burden was predictive for overall survival when prostate radiotherapy was used [1], with increased overall survival for those patients with <= 3 metastases, with no specific location of importance (<2% of patients had >= 4 bone metastases confined within the vertebral column):

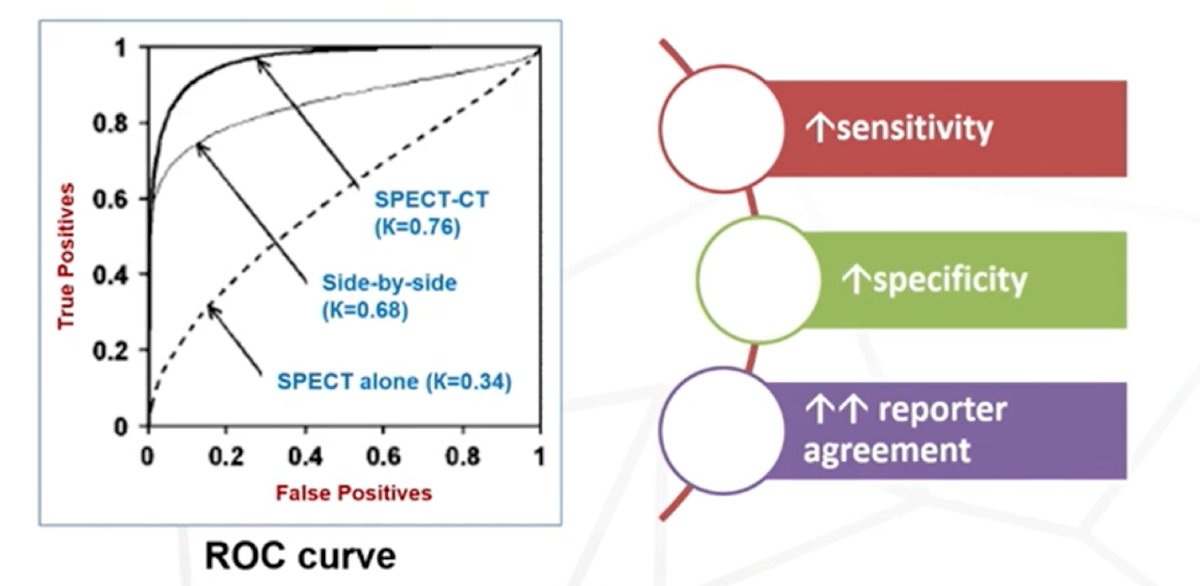
If PSMA PET/CT is not available, Dr. Hofman encourages the use of SPECT-CT, which has shown improved detection compared to SPECT versus side-by-side SPECT + CT:
Dr. Hofman emphasized that more accurate imaging is not stage migration. So, how much more accurate is PSMA PET/CT? Based on data from the proPSMA trial [2], PSMA PET/CT has 27% greater accuracy than conventional imaging (95% CI 23-31%; p < 0.001):

Additionally, PSMA PET/CT offers further granularity with regards to equivocal studies, decreasing the number of false positives in the proPSMA study:

One may wonder if false positive results on bone scan/CT scan could be driving the overall survival benefit of radiotherapy in metastatic disease, however if we use the Ali et al. [1] analysis of STAMPEDE Arm H as an example, patients with >= 3 bone metastasis are true positives and truly have M1 disease, thus false positives driving a survival benefit would be unlikely with increasing number of bone lesions:

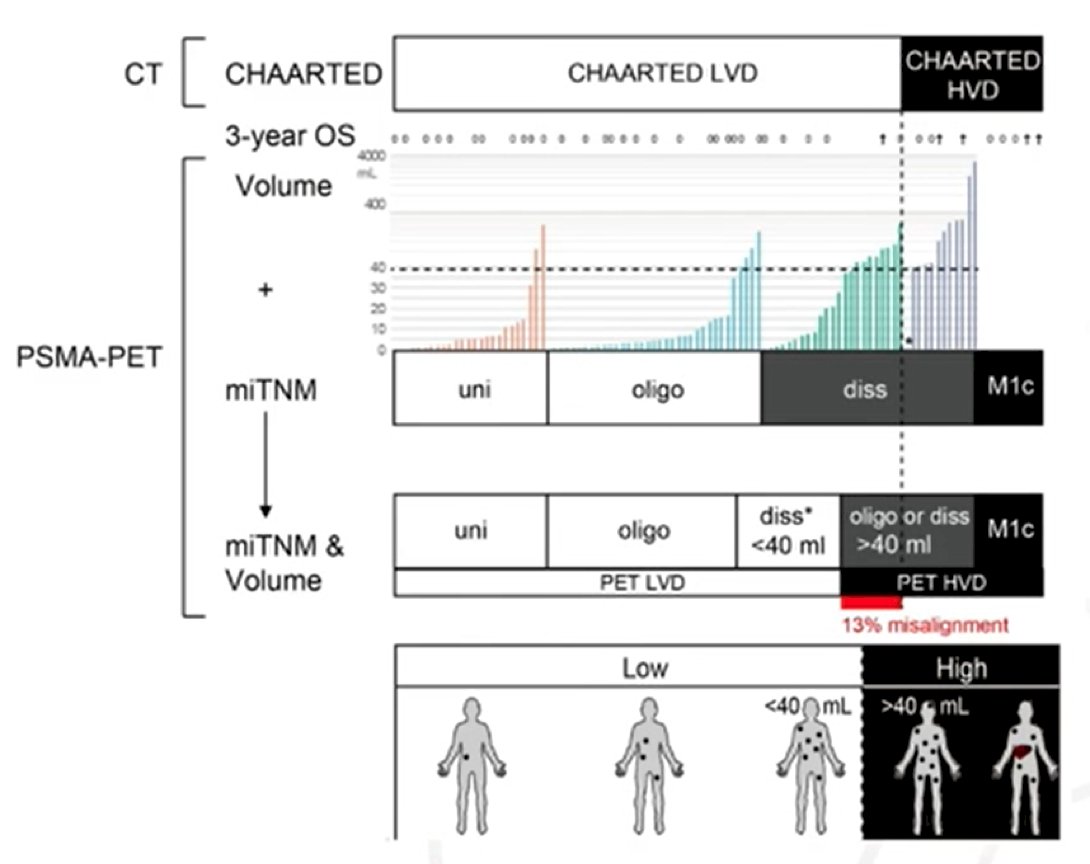
Perhaps most importantly, Dr. Hofman suggests that we need to move away from high vs low volume disease, number of bone lesions, etc and ultimately use quantitative total tumor volume with PSMA PET/CT:
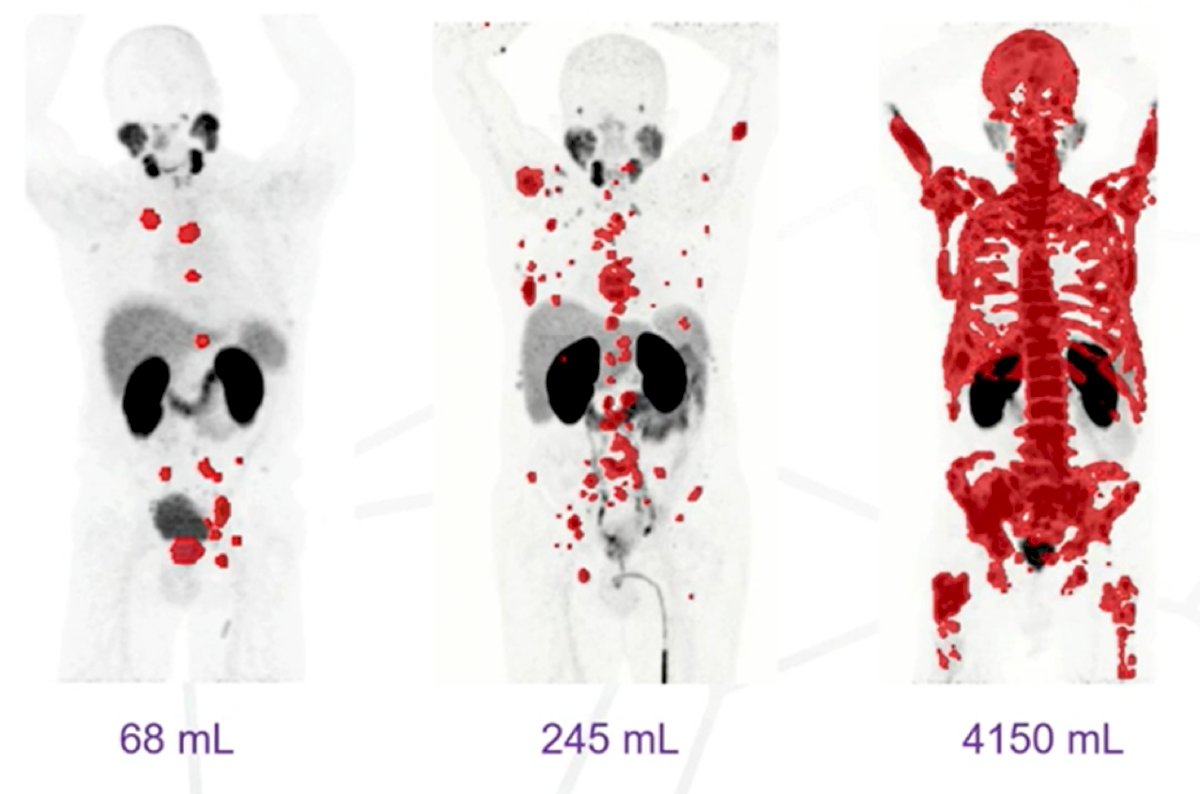
Barbato et al. [3] have previously used PSMA PET/CT for the assessment of mHSPC volume. This study included 85 patients with CT-based CHAARTED-low volume disease and 20 CT-based CHAARTED-high volume disease. A PSMA-tumor volume of ~40 ml was the optimal cutoff between CT-based CHAARTED-low volume disease (non-unifocal) and high volume disease (non-M1c), with an AUC of 0.86. Stratification into PET-low volume disease (unifocal or oligometastatic/disseminated <~40 mL) and PET-high volume disease (oligometastatic/disseminated ≥~40 mL or M1c) had 13% misalignment with CHAARTED criteria:
Dr. Hofman concluded his presentation by suggesting that technological advances have outpaced “evidence base”, as well as highlighting the following summary points:
- We should not make wrong decisions using 2D planar bone scans
- More accurate imaging is not stage migration
- We should not extrapolate data presented in this presentation to the mCRPC disease space
Presented By: Michael Hofman, MBBS (Hons), FRACP, FAANMS, FICIS, Molecular Imaging & Therapeutic Nuclear Medicine, Peter MacCallum Cancer Center, The University of Melbourne, Melbourne, Australia
Written By: Gina B. Carithers, UroToday.com during the 2022 Advanced Prostate Cancer Consensus Conference (APCCC) Annual Hybrid Meeting, Lugano, Switzerland, Thurs, Apr 28 – Sat, Apr 30, 2022.
References:
- Ali A, Hoyle A, Haran AM, et al. Association of bone metastatic burden with survival benefit from prostate radiotherapy in patients with newly diagnosed metastatic prostate cancer: A secondary analysis of a randomized clinical trial. JAMA Oncol. 2021 Apr 1;7(4):555-563.
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.
- Barbato F, Fendler WP, Rauscher I, et al. PSMA-PET for the assessment of metastatic hormone-sensitive prostate cancer volume of disease. J Nucl Med 2021 May 14;62(12):1747-1750.


