(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) held in Lugano, Switzerland between April 25th and 27th was host to a high-risk and locally advanced prostate cancer session. Dr. Declan Murphy discussed whether the use of digital rectal examination for defining local T-stage is still appropriate during the current era of next-generation and magnetic resonance imaging (MRI).
Before discussing and debating the potential clinical utility and additional information provided by a digital rectal examination (DRE), we need to consider patient preferences and attitudes toward DRE in clinical practice. Fear of DRE can be a significant factor in men not talking about prostate cancer. In a Prostate Cancer UK Survey of 2,000 men, 60% noted that they were concerned about a DRE and 37% reported they would not speak to a general practitioner about prostate issues because of such fear. Notably, Black men reported a higher cultural stigma around DRE, despite these men being at higher risk of prostate cancer-related mortality.1
Dr. Murphy noted that ultimately, the whole discussion on the value of a DRE depends on the availability of multi-parametric MRI (mpMRI), which is often dictated by which part of the world the clinician and patient live in.
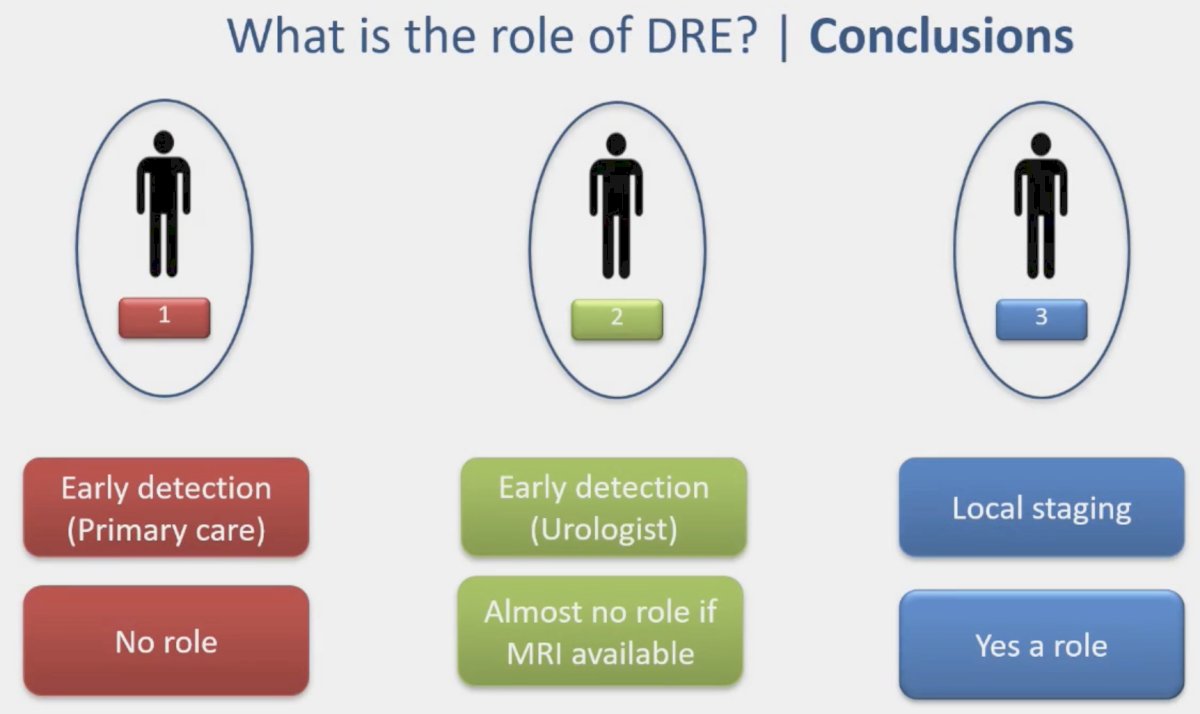
The role/value of DRE can be considered across three scenarios:
- Early detection (primary care)
- Early detection (urologist)
- Local staging
In the primary care setting, this exam is often performed in a 50- to 70-year-old asymptomatic male at average risk of prostate cancer. While MRI is usually not available in this setting, which would in theory leverage the role of DRE in such cases, DRE has poor sensitivity for detecting malignancies and the experience of the primary care physician for performing DREs is often variable, limiting its utility. Additionally, patients may be hesitant to undergo a DRE, further diminishing its value. The proponents of DRE will argue that DRE may detect aggressive low PSA tumors (~1-2%), however, Dr. Murphy noted that this does not necessarily justify performing a DRE in all such men and cited two recent papers that have ‘kill off’ the value DRE in this setting.
In a systematic review and meta-analysis of 8 prospective studies, including 85,738 participants, Matsukawa et al. demonstrated that DRE had a similar positive predictive value (0.21 – 0.22) to PSA, and there was no additional positive predictive value benefit to combining the two tests. Furthermore, DRE had a lower cancer detection rate, compared to PSA (0.01 versus 0.03).2 The 2024 PROBASE trial of 46,000 men aged ≥45 years recently published in European Urology demonstrated that only 57 men had suspicious DRE findings, of whom only 3 had cancer detected (0.03% of the population). PSA-based screening led to a four-fold higher detection rate. Notably, 86% of men with detected cancers had normal DRE findings.3 As such, it becomes clear based on these two recent studies that DRE has poor diagnostic performance in the primary care setting.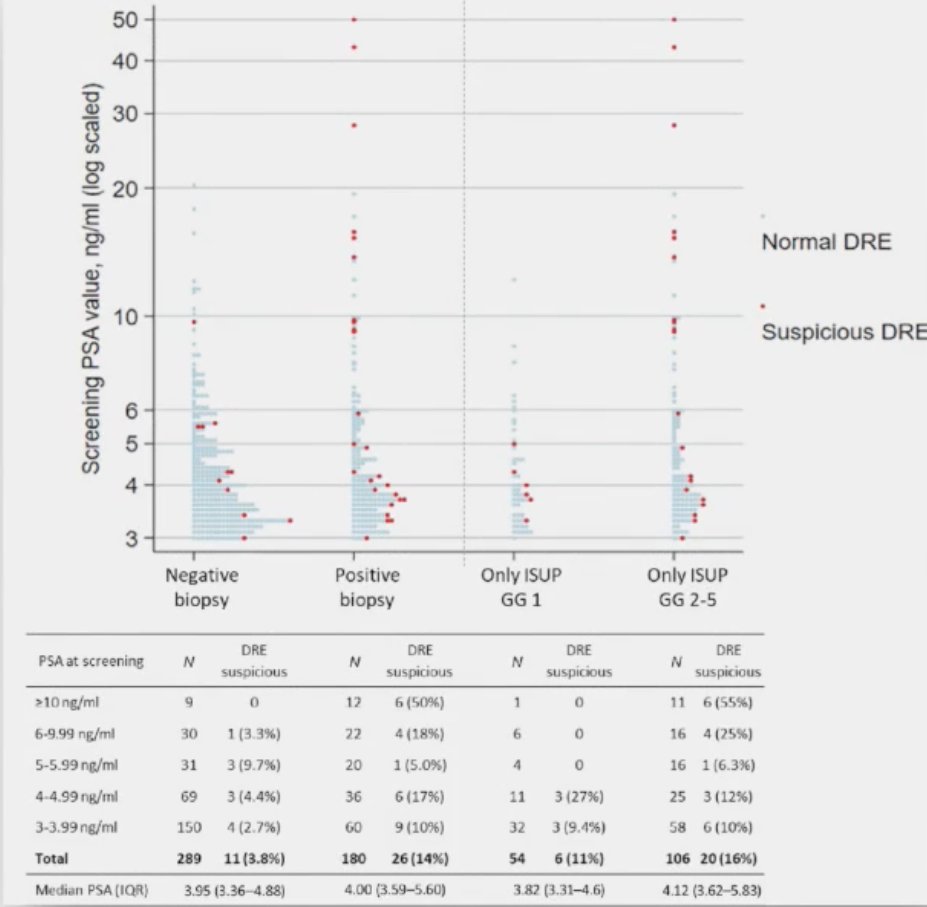
What about early detection for urologists? In the current era of MRI-guided biopsy decision making and targeted sampling, it is clear that MRI plays a major role in improving the detection of clinically significant cancer while minimizing the detection of Grade Group 1 disease. In the PRECISION trial, men with a clinical suspicion of prostate cancer who had not previously undergone a prostate biopsy were randomized to undergo MRI, with or without targeted biopsy, or standard transrectal ultrasonography-guided biopsy. Men in the MRI-targeted biopsy group underwent a targeted biopsy (without standard biopsy cores) if the MRI was suggestive of prostate cancer; men whose MRI results were not suggestive of prostate cancer were not offered biopsy. Standard biopsy was a 10-to-12–core, transrectal ultrasonography-guided biopsy. Notably, 15% of men in this trial had an ‘abnormal’ DRE.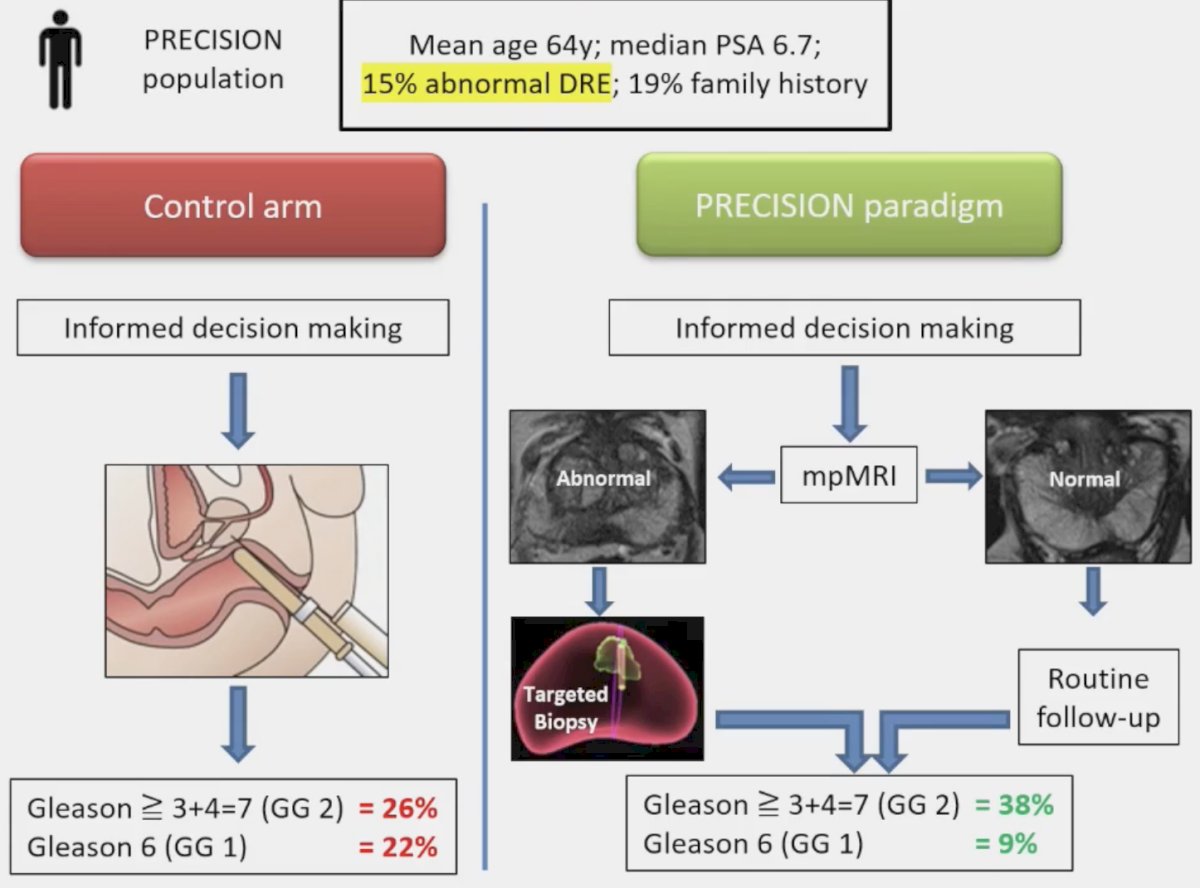
Men in the MRI group had increased detection of ≥Grade Group 2 disease (38% versus 26%) with lower detection of Grade Group 1 disease (22% versus 9%). Notably, 28% of men avoided a biopsy with MRI, and a median of only 4 cores were obtained with such a targeted approach. Dr. Murphy argued that these results are an overwhelming ‘win’ for MRI and ‘drown out’ any potential benefits for DRE in this setting. Based on the results of this trial, among many others, The Lancet Commission on Prostate Cancer currently notes that PSA testing needs to be linked to MRI-based assessment and treatment only for high-grade tumors, which would mitigate overdiagnosis and overtreatment.4
Dr. Murphy offered his opinion that DRE has little role for urologists who use MRI in early detection: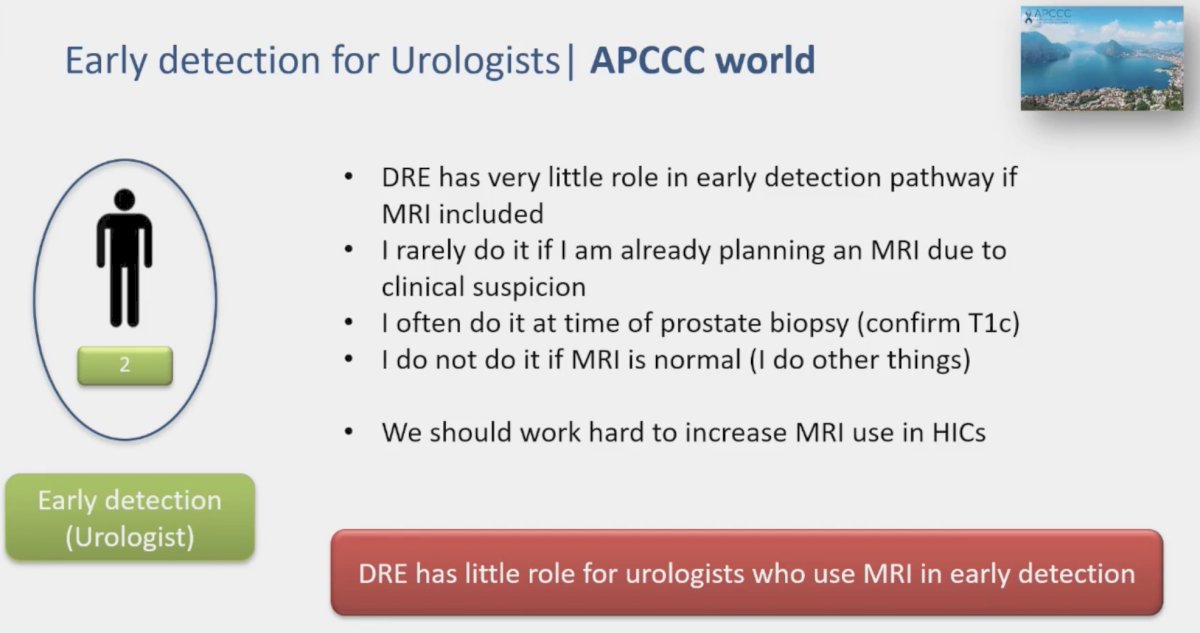
What about the use of DRE for local staging? DRE remains an important tool for local staging if MRI is not available and a key component of conventional TNM risk stratification systems. It also may help determine resectability of a tumor. Furthermore, MRI is often unavailable in the real world and CT performs poorly for local staging. As such, in this setting, Dr. Murphy argued that DRE still has a key role if MRI is unavailable.
There remains debate as to whether the results of MRI or DRE should be used to clinically stage patients. While the clinical stage in risk stratification systems is reliant on DRE findings, DRE is often inaccurate compared to MRI. In the example below, the patient has cT2 per DRE, but the MRI suggests the presence of T3 disease. What should this patient be staged as?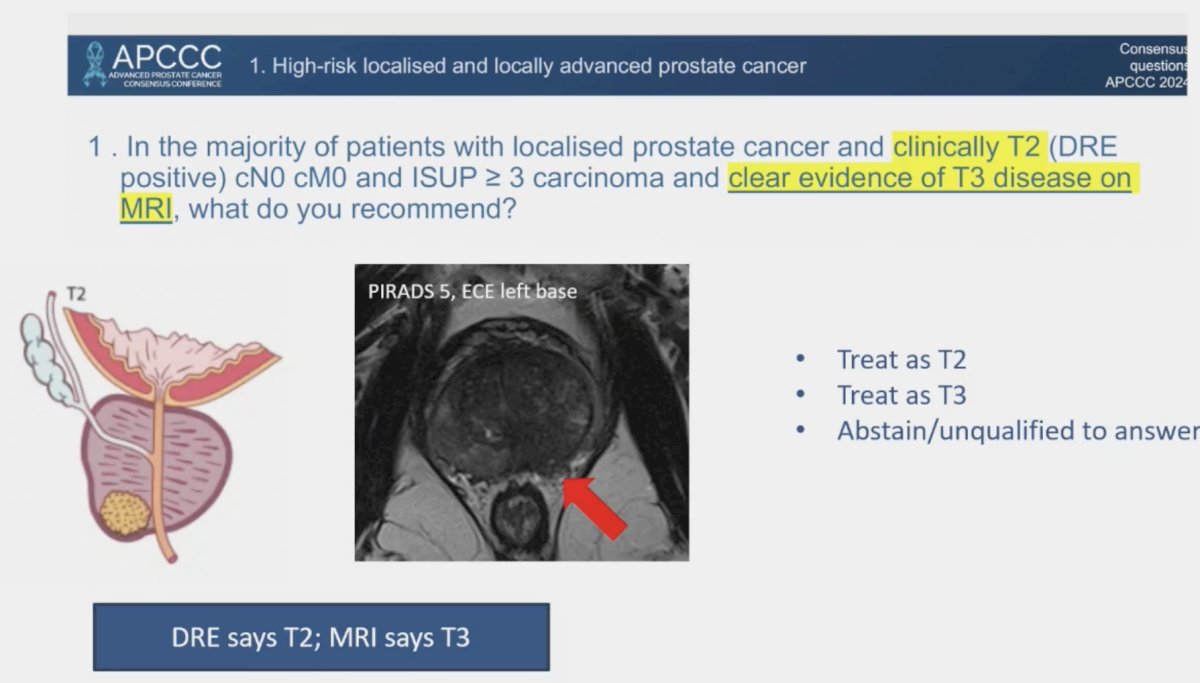
Dr. Murphy highlighted the emerging role of PSMA PET/CT for the diagnosis of prostate cancer, although not advocating for its routine use in this setting. The PRIMARY trial was a prospective multicenter phase II imaging trial that enrolled men with suspected prostate cancer, no prior biopsy, and a recent mpMRI examination within 6 months, and for whom prostate biopsy was planned. In total, 291 men underwent an mpMRI, 68Ga-PSMA PET/CT, and systematic biopsy with or without targeted biopsy.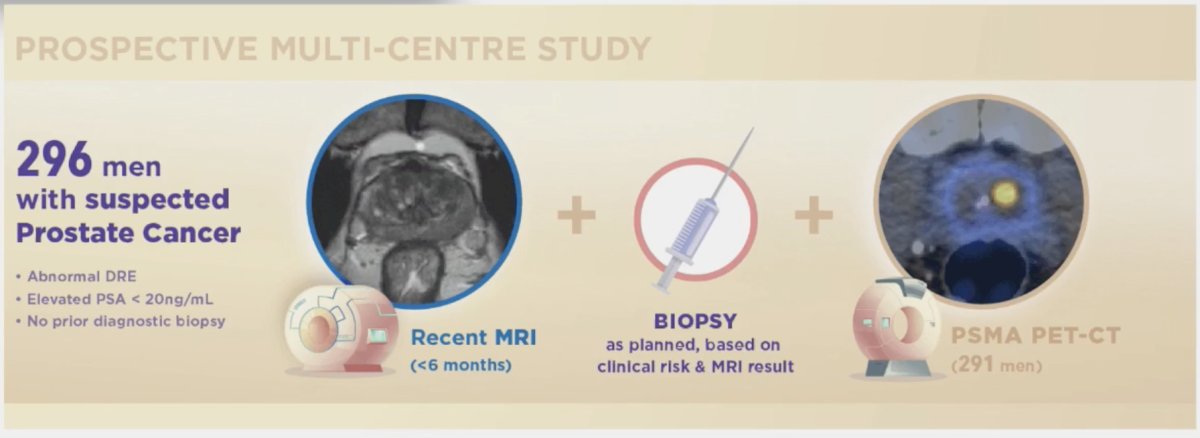
A combined mpRMI + PSMA-PET/CT approach improved the sensitivity from 83% with MRI alone to 97% when combined (NPV: 72% to 91%), at the expense of decreased specificity (53% reduced to 40%). Significantly, a combination approach reduced the false negative rate for detection of clinically significant prostate cancer from 17% to 3.1%.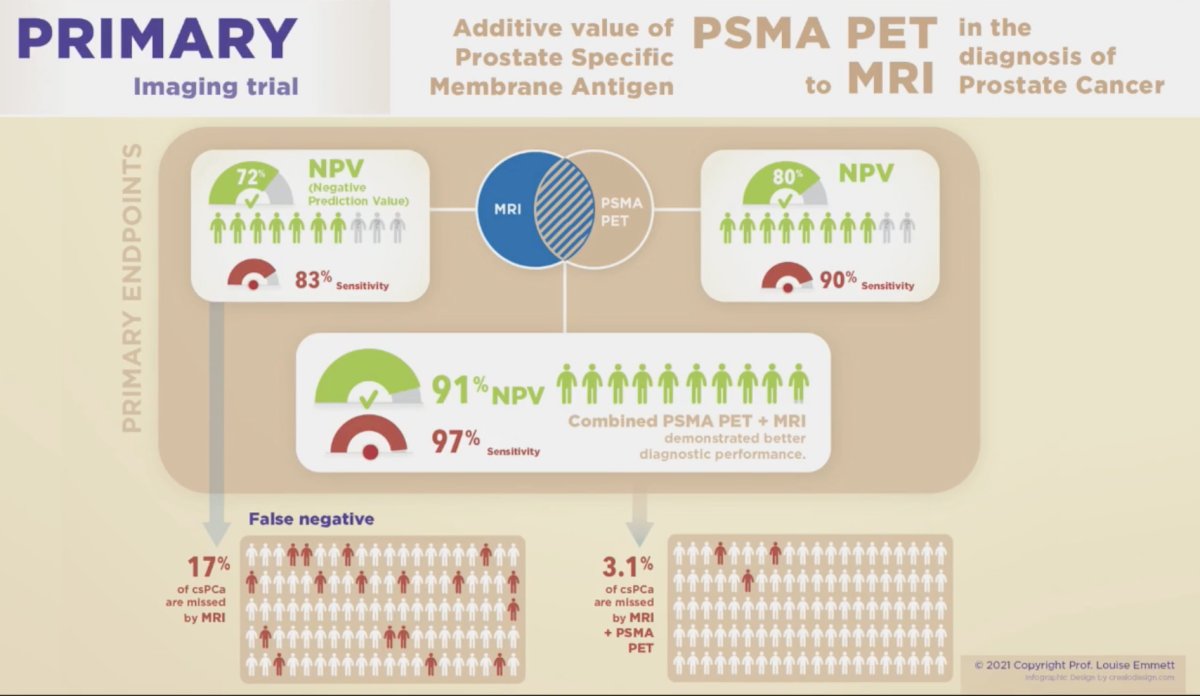
The proportion of men who could safely avoid a biopsy with a negative PSMA PET + MRI was 19% among all patients and 38% among those with PIRADS 2–3. Interestingly, there was a direct correlation between the SUVmax level and increased/worsening ISUP grade group disease. The probability of clinically significant prostate cancer increased exponentially as the SUVmax increased from 2.5 to 10, with the probability of such disease leveling off at 1.0 for lesions/patients with SUVmax of 10 or greater.5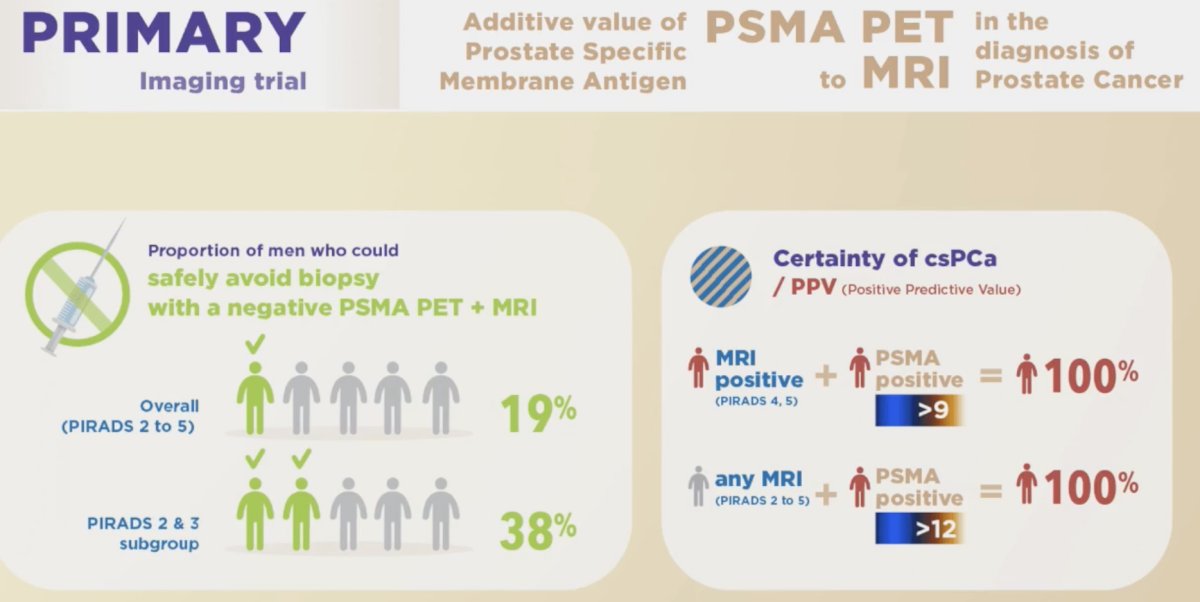
Dr. Murphy concluded his presentation with the following take-home messages regarding the role of DRE:
- Early detection in the primary care setting No role
- Early detection in the urologist office setting Almost no role if MRI is available
- Local staging Yes, there is a role
Presented by: Declan G. Murphy, MD, FRACS, FRCS, Professor, Consultant Urologist, Direct of Genitourinary Oncology and Robotic Surgery, Peter MacCallum Cancer Centre, Melbourne, Australia
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference, Lugano, Switzerland, April 25th – April 27th, 2024
References:
- Kirby M, Merriel SWD, Olajide O, et al. Is the digital rectal exam any good as a prostate cancer screening test? Br J Gen Pract. 2024;74(740): 137-139.
- Matsukawa A, Yanagisawa T, Bekku K, et al. Comparing the Performance of Digital Rectal Examination and Prostate-Specific Antigen as a Screening Test for Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol Oncol. 2024:S2588-9311(23)00292-4.
- Boschheidgen M, Albers P, Schlemmer H, et al. Multiparametric Magnetic Resonance Imaging in Prostate Cancer Screening at the Age of 45 Years: Results from the First Screening Round of the PROBASE Trial. Eur Urol. 2024;85(2): 105-11.
- James ND, Tannock I, N’Dow J, et al. The Lancet Commission on prostate cancer: planning for the surge in cases. Lancet. 2024: S0140-6736(24)00651-2.
- Emmett L, Buteau J, Papa N, et al. The Additive Diagnostic Value of Prostate-specific Membrane Antigen Positron Emission Tomography Computed Tomography to Multiparametric Magnetic Resonance Imaging Triage in the Diagnosis of Prostate Cancer (PRIMARY): A Prospective Multicentre Study. Eur Urol. 2021;80(6): 682-9.


