(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on the treatment for biochemical recurrence/PSA persistence, and a presentation by Dr. Bertrand Tombal discussing patients with high-risk first biochemical recurrence after radical prostatectomy who are candidates for systemic therapy alone without local salvage radiotherapy. Dr. Tombal notes that in EAU high risk biochemical recurrence patients, these patients are currently staged with a PSMA PET/CT scan. If there is local or locoregional disease, everything is irradiated “ad nauseam”. If there is distant disease, these patients are treated with systemic therapy. The EAU guidelines state that for patients with biochemical recurrence after prostatectomy, patients should be offered early salvage intensity-modulated radiotherapy/volumetric arc radiation therapy plus image-guided radiotherapy to men with two consecutive PSA rises (Strength rating: Strong). However, Dr. Tombal questions whether this statement should, in fact, have a strong rating.
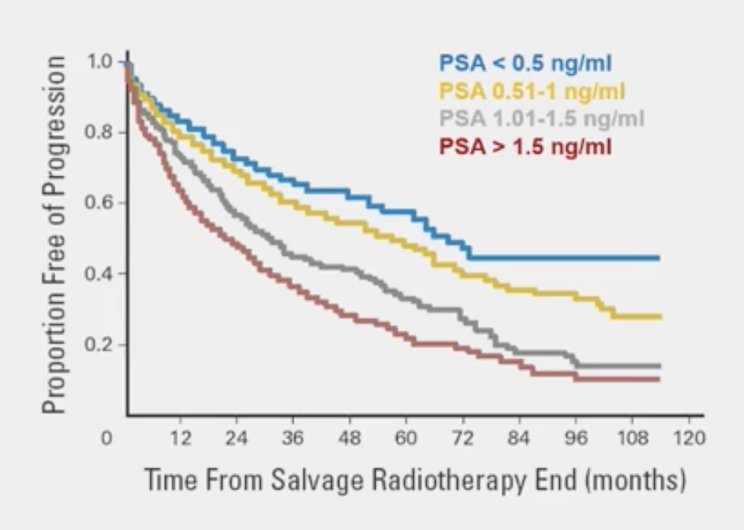
Salvage radiotherapy is an option for recurrence of prostate cancer after radical prostatectomy. In 2004, Stephenson et al.1 assessed 501 patients who received salvage radiotherapy for detectable PSA after radical prostatectomy, with the goal of delineating patients who may benefit from salvage radiotherapy. Over a median follow-up of 45 months, 250 patients (50%) experienced disease progression after treatment, 49 (10%) developed distant metastases, 20 (4%) died from prostate cancer, and 21 (4%) died from other or unknown causes. The 4-year progression-free probability was 45% (95% CI, 40%-50%). The proportion free of progression stratified by PSA is as follows:
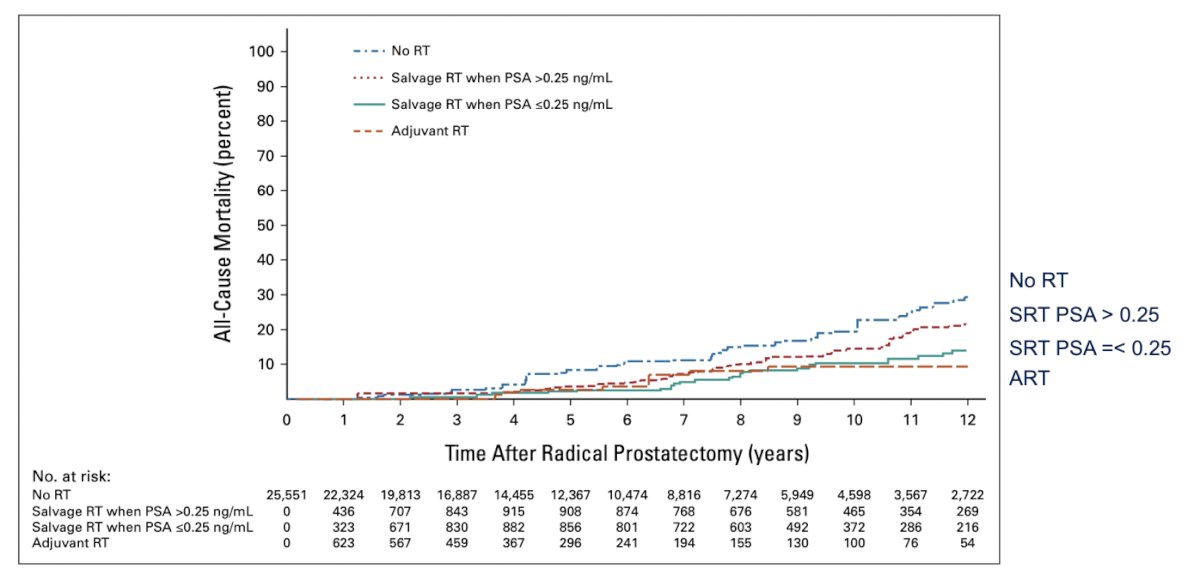
Salvage radiotherapy has been considered the only potentially curative therapy after biochemical failure and has been associated with better outcomes if given at lower PSA levels. Tilki and colleagues showed that salvage radiotherapy when given at a PSA equal or lower than 0.25 ng/mL is associated with improved all cancer-mortality2:
Early salvage radiotherapy provides the best possibility of cure for patients with an increasing PSA after radiotherapy. The RAVES and RADICAL trials assessing salvage radiotherapy in post-radical prostatectomy patients with PSA levels exceeding 0.1-0.2 ng/mL showed 5-year freedom from biochemical recurrence and biochemical recurrence free survival rates of 88%. However, although biochemical progression is now widely accepted as a surrogate marker of prostate cancer recurrence, work from Dr. Spratt’s group3 suggests that intermediate clinical endpoints based on biochemical and local failure did not meet the second condition of the meta-analytical approach and are not surrogate endpoints for overall survival in localized prostate cancer.
Dr. Tombal emphasized that there is no randomized controlled trial that has demonstrated that applying prostate bed radiotherapy, metastasis directed therapy, or both significantly delays metastasis free survival or overall survival versus observation. Referring again to the Stephenson et al. study, Dr. Tombal notes that EAU high-risk patients do not do well with salvage radiotherapy. The following are predictors of PSA progression after salvage radiotherapy1:
- Gleason score 8-10: HR 2.6, 95% CI 1.7 – 4.1
- Pre-radiotherapy PSA level > 2.0 ng/mL: HR 2.3, 95% CI 1.7 – 3.2
- PSA doubling time <= 10 months: HR 1.7, 95% CI 1.2 – 2.2
Dal Pra et al.4 previously validated the Decipher genomic classifier in patients receiving salvage radiotherapy without ADT after radical prostatectomy. They conducted an analysis of the SAKK 09/10 trial assessing 350 men with biochemical recurrence after radical prostatectomy who received salvage radiotherapy (64 – 70 Gy) without concurrent hormonal therapy or pelvic nodal radiotherapy. The primary endpoint was biochemical progression, whereas secondary endpoints were clinical progression and time to hormone therapy. The analytic cohort included 226 patients, with a median follow-up of 6.3 years. The Decipher genomic classifier score (high versus low-intermediate) was independently associated with the rates of biochemical progression (sHR 2.26, 95% CI 1.42 - 3.60; p < 0.001), clinical progression (HR 2.29, 95% CI 1.32 - 3.98; p = 0.003), and use of hormone therapy (sHR 2.99, 95% CI 1.55 - 5.76; p = 0.001).
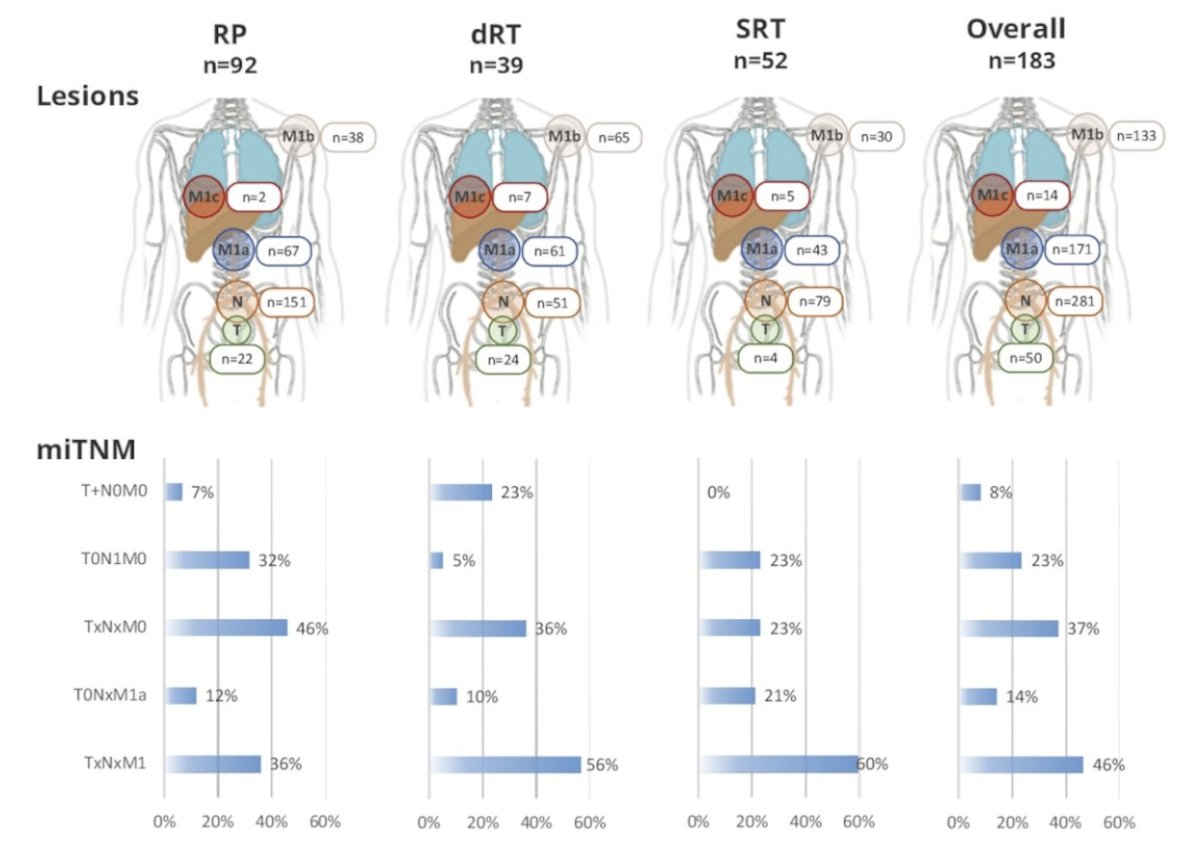
Dr. Tombal notes that based on the EAU guidelines, for patients with a PSA recurrence after radical prostatectomy, we should perform a PSMA PET/CT if the PSA level is > 0.2 ng/mL and if the results will influence subsequent treatment decisions (Strength rating: Weak). At ASCO 2023, Dr. Armstrong presented PSMA PET/CT findings in an “EMBARK-like” cohort of 183 patients with high-risk non-metastatic hormone sensitive prostate cancer. Median pre-scan PSA levels and PSA doubling time in patients who underwent radical prostatectomy (n = 92), definitive radiotherapy (n=39), post-radical prostatectomy salvage radiotherapy (n = 52), and the overall cohort (n = 183) were 2.4 ng/mL (IQR 1.4-4.8), 6.9 ng/mL (IQR 3.5-18.5), 2.7 ng/ml (IQR 1.7-5.3), 2.8 ng/mL (IQR 1.7-6.7), respectively, and 3.1 months (IQR 1.9-5.3), 3.2 months (IQR 2.1-4.8), 4 months (IQR 2.6-5.4), 3.6 months (IQR 1.9-5.3), respectively. Overall, 85.2% of patients were PSMA PET positive, with 609 total PSMA PET positive lesions, and 3.9 mean number of lesions per case. The following highlights the lesion and miTNM staging distributions by treatment modality:
Dr. Tombal continued his presentation by highlighting several additional thoughts based on the current state of biochemical recurrence:
- The only hormone that increases overall survival in the biochemical recurrence setting is bicalutamide in the late salvage setting (PSA > 0.7 ng/mL)
- Patients with high-risk features, and those with distant lesions on PSMA PET do not do well with salvage radiotherapy, and they need ADT anyway
- One of the main justifications for radiotherapy on the prostate bed, pelvis, or metastasis was to delay systemic treatment
Dr. Tombal then highlighted the TOAD trial, which assessed when to initiate ADT in patients with biochemical recurrence.5 This was a phase III randomized trial that randomized 293 men to immediate ADT vs deferred ADT (delay of at least 2 years). Over a median follow-up of 5 years, among patients with biochemical relapse there was no significant difference in overall survival (HR 0.58, 95% CI 0.30-1.12, p = 0.10):
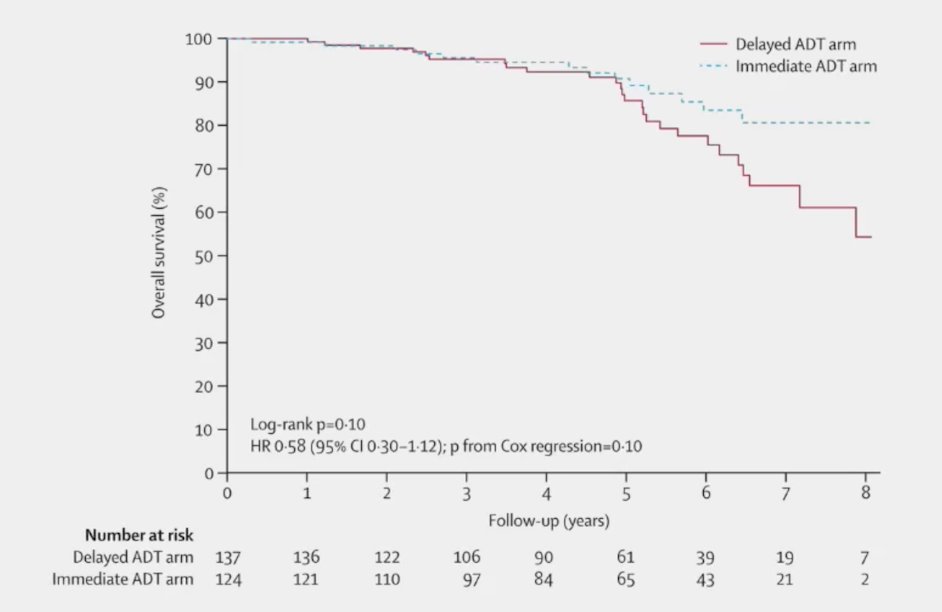
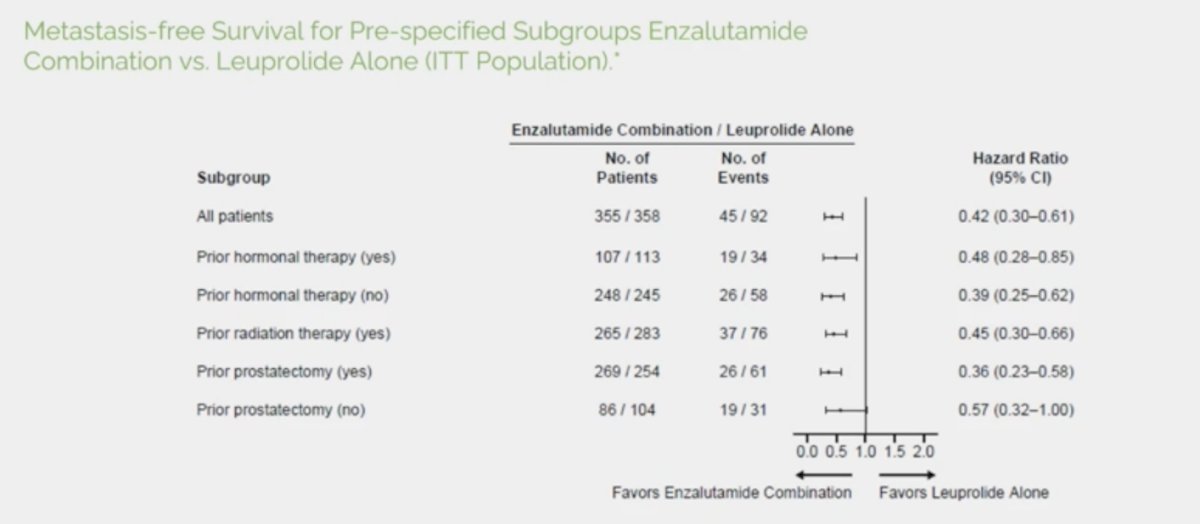
Dr. Tombal notes that it was acceptable to delay systemic treatment with ADT since studies have failed to show that it significantly increases overall survival but negatively impacts quality of life. Until 2023, when, notably, enzalutamide +/- ADT was shown to be the only treatment demonstrating a substantial benefit in metastasis free survival compared to ADT in a large randomized trial. This is true provided that the patient is truly an “EMBARK patient” (PSA > 1 ng/mL and PSA doubling time < 9 months). Additionally, metastasis free survival in EMBARK showed benefit in all key subgroups:
So, is it still acceptable to delay systemic treatment after EMBARK?
Dr. Tombal concluded his presentation by emphasizing the patients with high-risk first BCR after radical prostatectomy that are candidates for systemic therapy alone without local salvage radiotherapy:
- All of them
- This is not a discussion about salvage radiotherapy +/- short or long course of ADT
- It is now a matter of short-course ARTA +/- salvage radiotherapy
- The benefit of the latter in this setting is yet to be proven
Presented by: Bertrand Tombal, MD, PhD, Institut de Recherche Clinique, Université Catholique de Louvain, Brussels, Belgium
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:
- Stephenson AJ, Shariat SF, Zelefsky MJ, et al. Salvage radiotherapy for recurrent prostate cancer after radical prostatectomy. JAMA. 2004 Mar 17;29(11):1325-1332.
- Tilki D, Chen MH, Wu J, et al. Prostate-Specific Antigen Level at the Time of Salvage Therapy After Radical Prostatectomy for Prostate Cancer and the Risk of Death. J Clin Oncol. 2023 May 1;41(13):2428-2435.
- Gharzai LA, Jiang R, Wallington D, et al. Intermediate clinical endpoints for surrogacy in localized prostate cancer: An aggregate meta-analysis. Lancet Oncol. 2021 Mar;22(3):402-410.
- Dal Pra A, Ghadjar P, Hayoz S, et al. Validation of the Decipher genomic classifier in patients receiving salvage radiotherapy without hormone therapy after radical prostatectomy - an ancillary study of the SAKK 09/10 randomized clinical trial. Ann Oncol. 2022;33(9):950-958.
- Duchesne GM, Woo HH, Bassett JK, et al. Timing of androgen-deprivation therapy in patients with prostate cancer with a rising PSA (TROG 03.06 and VCOG PR 01-03 [TOAD]): A randomized, multicentre, non-blinded, phase 3 trial. Lancet Oncol 2016;17(6):727-737.
Related Content:


