(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) held in Lugano, Switzerland between April 25th and 27th was host to a high-risk and locally advanced prostate cancer session. Dr. Alberto Briganti debated in favor of surgery, as part of a multimodal regimen, as the best approach to manage a fit patient with high-risk, localized, or locally advanced prostate cancer.
Why should we consider surgery for such patients? Post-operative treatment can be tailored to the patient’s characteristics leading to potential treatment de-intensification. Surgery allows for the full pathologic assessment, whereby up to 30-50% of such patients may be found to harbor specimen-confined disease at surgical pathology. Adequate nodal treatment may be feasible with this approach, and radical prostatectomy may allow for maximization of local control. However, Dr. Briganti noted that strong evidence for surgery in this setting is non-existent. No randomized controlled trials of surgery have been specifically designed in this setting. Surgical treatment has side effects and select patients should receive radiotherapy anyway. It is also likely that surgery alone will not be curative, as patients will likely have a positive surgical margin.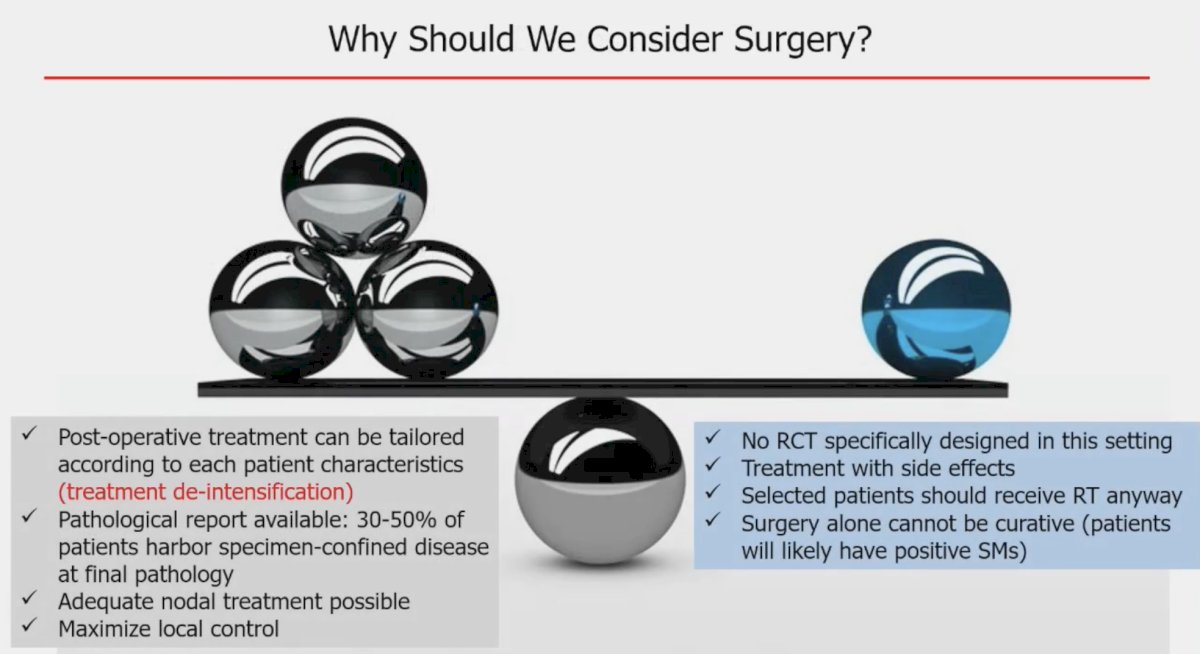
Current guidelines do not strongly endorse the use of radical prostatectomy in high-risk patients. As summarized below, the EAU guidelines note that radical prostatectomy can be offered to select patients as part of potential multi-modal therapy (weak recommendation). Additionally, there is no clear indication for pelvic lymph node dissections; but if performed, an extended template is recommended (strong recommendation). Dr. Briganti noted that current guidelines do not even mention radical prostatectomy for patients with cN1 disease.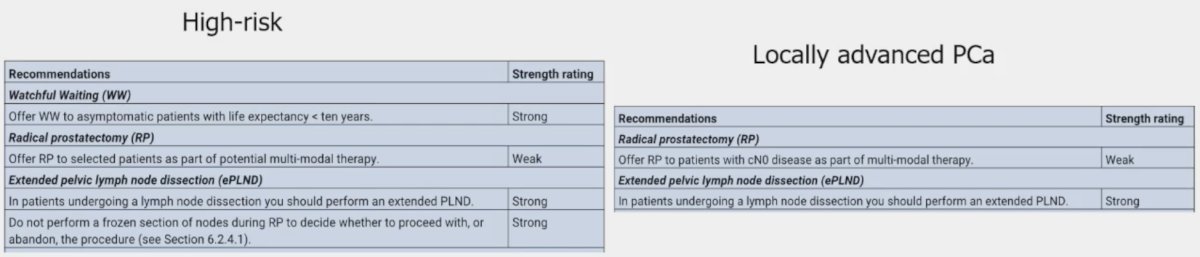
Dr. Briganti noted that it is hard to draw any firm conclusions from trials of radical prostatectomy in patients with localized disease given the inherent differences in the patient population characteristics and the historical nature of such trials. However, there appears to be minimal to no benefit for surgery versus watchful waiting/active monitoring/observation for patients with high-risk disease.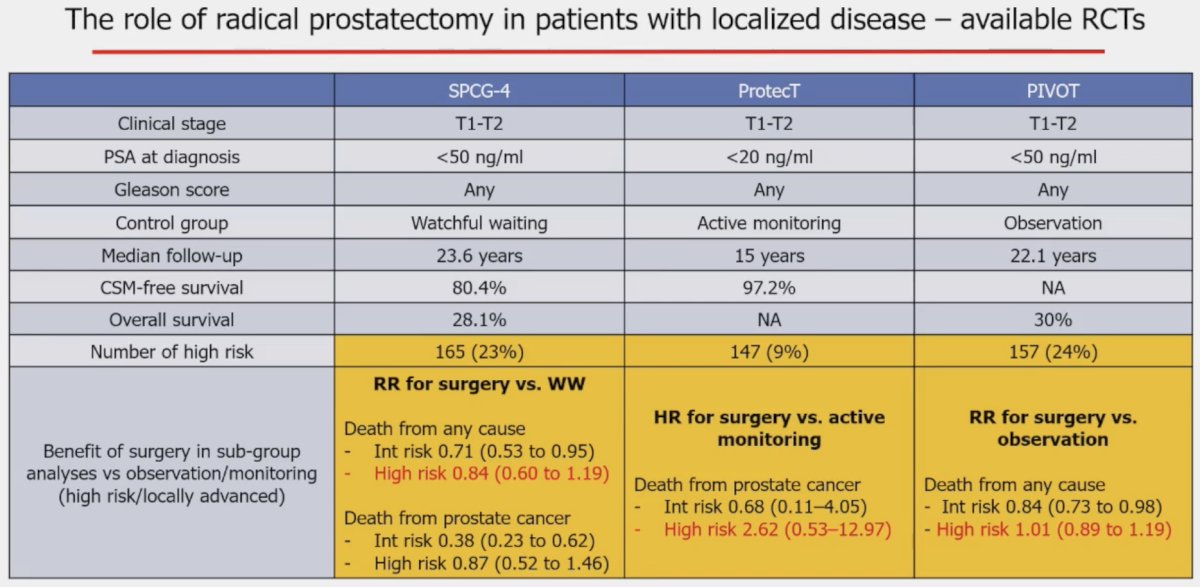
Can we tailor post-operative use of adjuvant treatments? Dr. Briganti noted that among 2,432 high-risk prostate cancer patients undergoing a radical prostatectomy plus an extended pelvic lymph node dissection, up to 20% have organ-confined disease (pT2N0R0-1) and 29% have specimen-confined disease (pT2-3aN0R0), with 10-year biochemical recurrence-free survivals of ~63%. As such, these patients could potentially be spared adjuvant therapy via a surgical pathology-tailored approach.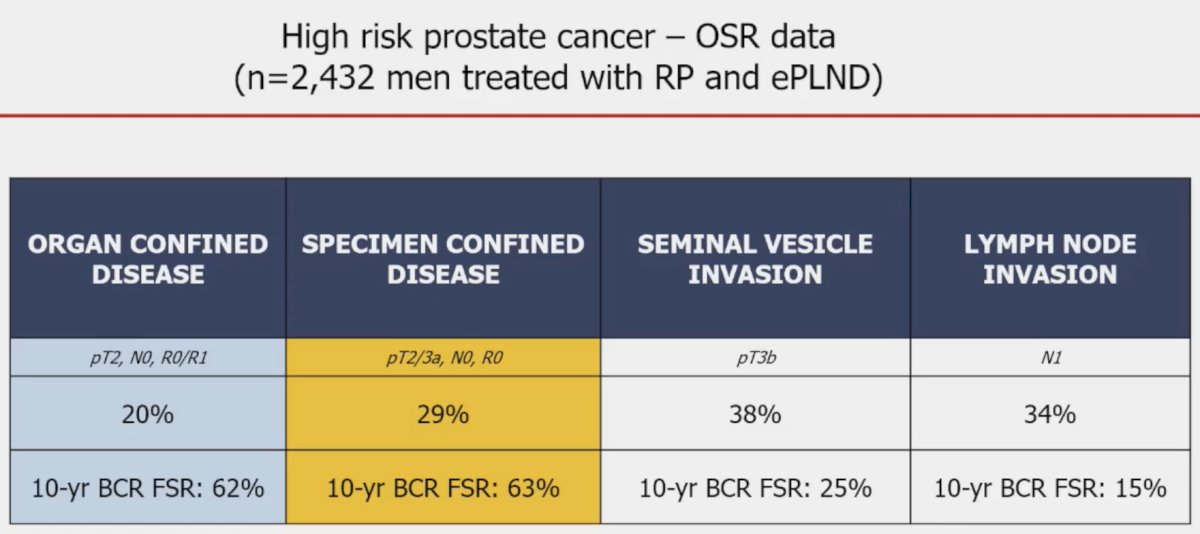
A promising aspect of surgical practice is that there appears to be a temporal reduction in positive surgical margins over more recent years in patients with high-risk/locally advanced disease. As shown below, surgical margin positivity has decreased from 39% in 2000/2001 to 26% in 2022/2023. Additionally, it is becoming more evident that unifocal, limited (<3 mm) positive margins are of low clinical significance, compared to the multifocal positive margins that portend worse cancer-specific and overall survivals.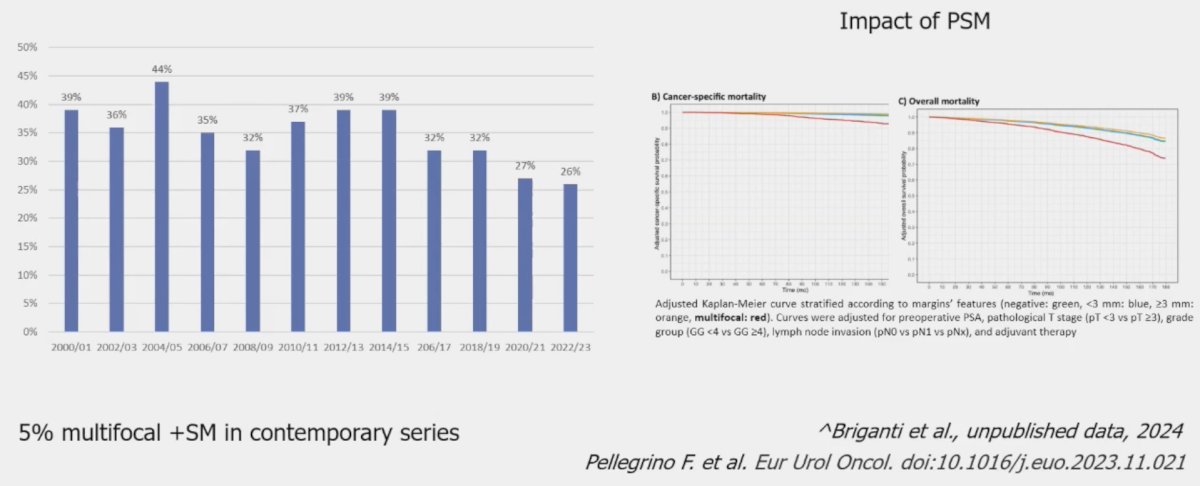
Extended pelvic lymph node dissections in high-risk patients demonstrate lymph node involvement rates of 22 to 44%. Can PSMA-PET/CTs be useful in these settings to exclude the presence of pathologic nodal involvement? The negative predictive value of PSMA-PET/CT is highly dependent on the pre-test risk of lymph node disease. The NPV of PSMA-PET/CT decreased from 98% to 84% as the risk of nodal involvement increases from 5% to 45%. In those studies where lymph node involvement prevalence ranged between 5 and 20%, the negative predictive value of PSMA PET/CT remained steadily above 90%.1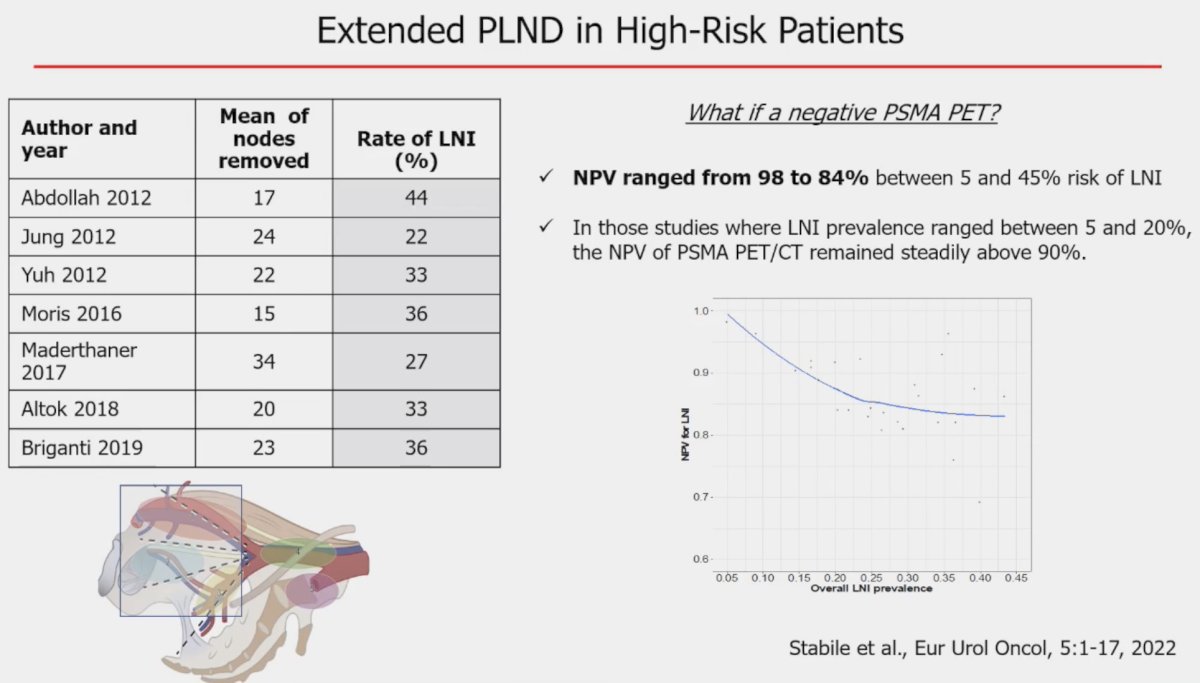
What about limited versus extended pelvic lymph node dissection. In the MSKCC trial initially published in 20212 and more recently updated at EAU 2024, Touijer et al. randomized 1,440 patients to limited versus extended pelvic lymph node dissection, respectively. The median number of nodes retrieved was 12 (IQR: 8-17) for the limited template and 14 (IQR 10-20) for the extended template. The corresponding rate of positive nodes was 12% and 14% (p = 0.3). Extended follow-up at a median of 4.2 years demonstrated no significant differences in the rate of biochemical recurrence. However, extended pelvic lymph node dissection reduced the incidence of metastases, including distant metastases. Notably, the greatest distant metastasis-free survival benefit effect appears to be present in patients with pathologic node-positive disease (HR: 0.49, 95% CI: 0.37-0.65, p<0.001).2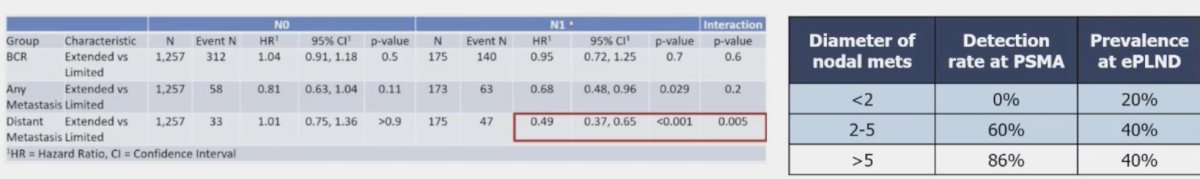
What about surgical therapy combined with other modalities such as neoadjuvant and/or adjuvant ADT? To date, there is no evidence to support the use of ADT in either setting for men who are candidates for surgery. This is reflected in the 2024 EAU guidelines, which strongly recommend against such practices.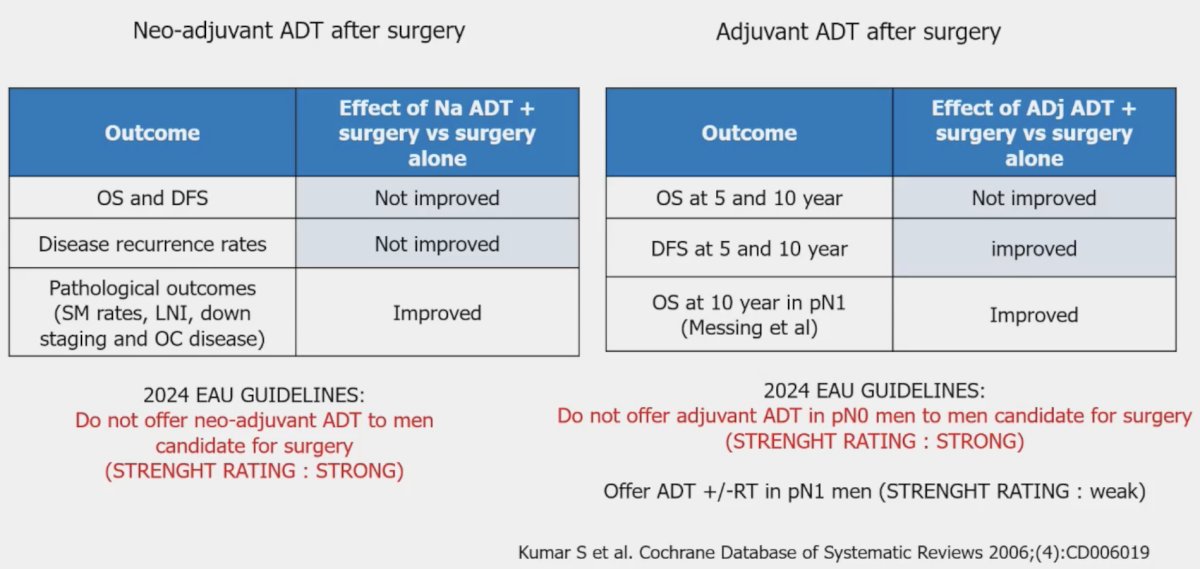
A similar story is seen with peri-operative chemotherapy with no strong evidence supporting such practice, although the Cancer and Leukemia Group B (CALGB) 90203 trial did demonstrate improved biochemical progression-free (HR: 0.69, 95% CI: 0.48–0.99), metastasis-free (HR: 0.70, 95% CI: 0.51–0.95), and overall survivals (HR: 0.61, 95% CI: 0.40–0.94) with neoadjuvant ADT + docetaxel.3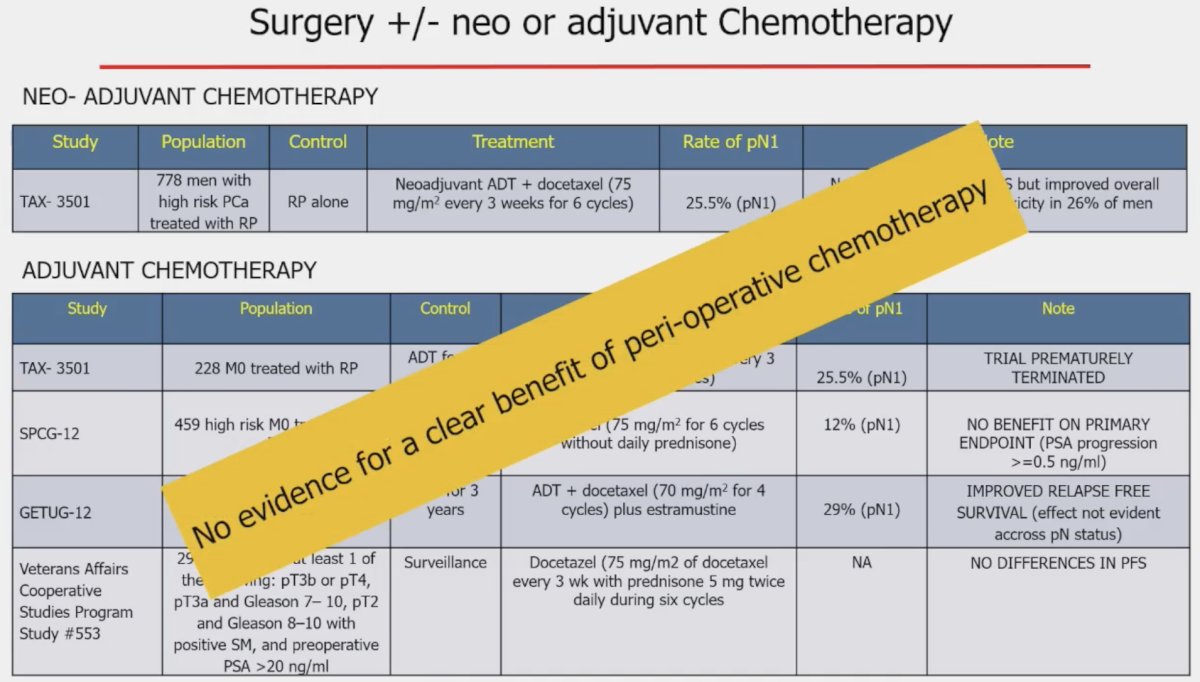
Dr. Briganti emphasized that use of surgery in these patients does not preclude post-operative radiotherapy, with an overall shift towards early salvage radiotherapy, as opposed to adjuvant radiotherapy, following the publication of RAVES, RADICALS-RT, and GETUG 17.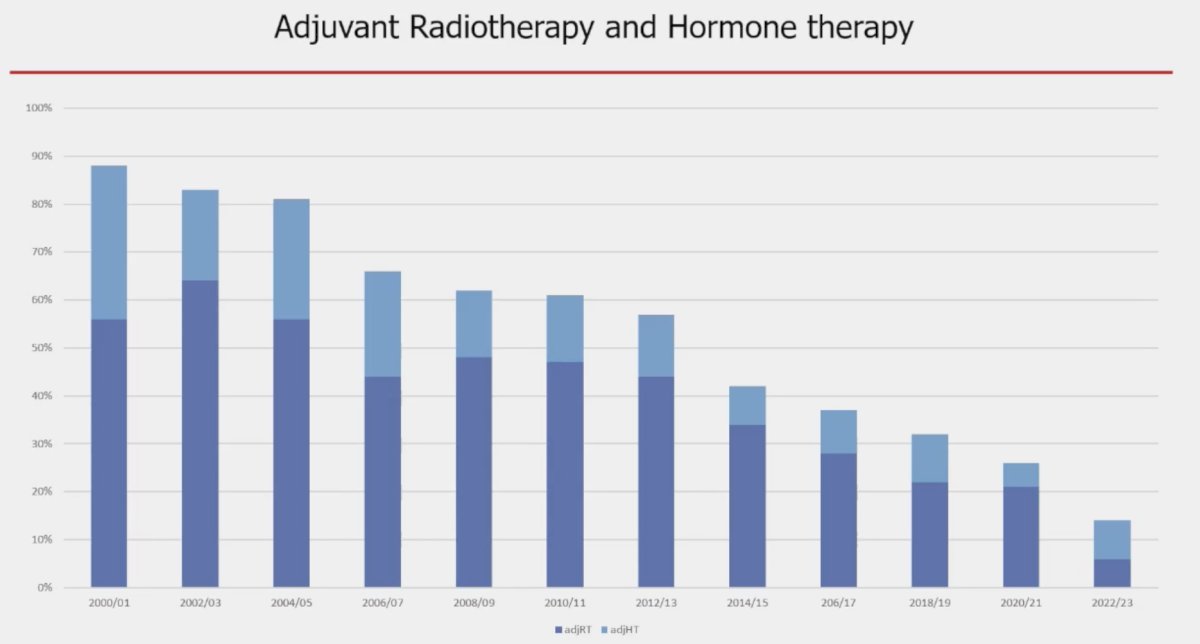
However, among pN0 patients with ISUP grade group 4-5 disease and pT3 +/- positive margins, the current EAU guidelines strongly recommend offering adjuvant radiotherapy, as opposed to early salvage radiotherapy.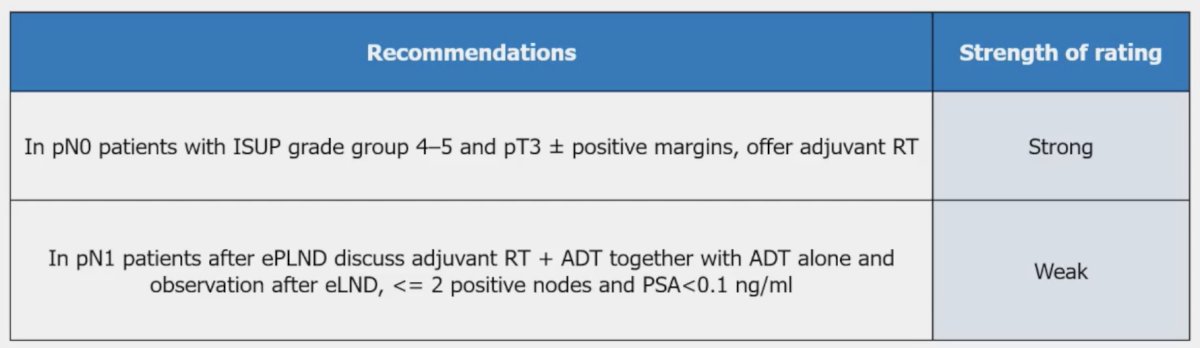
With regards to patients with cN1 disease, as previously mentioned, the current EAU guidelines do not even mention surgery for this patient population. However, Dr. Briganti noted that retrospective and population-based data support its use in this setting with comparable outcomes to radiotherapy + ADT, although comparisons to ‘triplet therapy’ with radiotherapy + ADT + abiraterone have not been performed to date. As for PSMA-PET/CT-detected cN1 disease, there remains a paucity of data regarding the role of surgery in these patients.
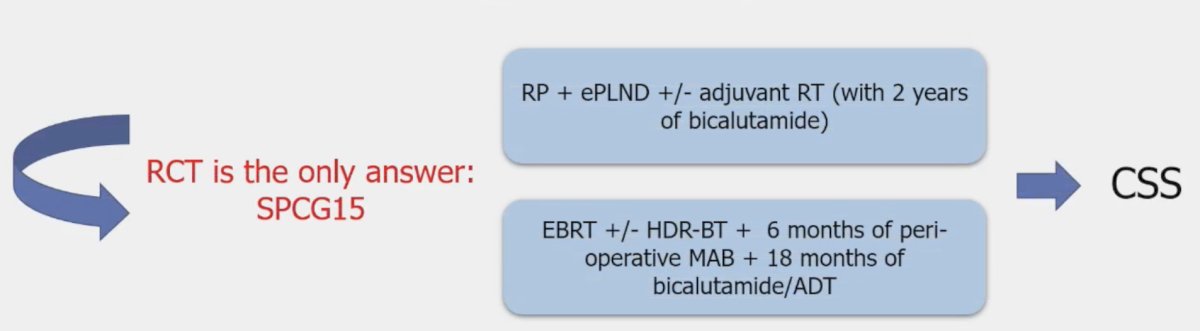
Dr. Briganti concluded his presentation noting the following with regard to surgery (+/- post-operative treatments) versus radiotherapy + ADT in high-risk patients:
- All current evidence is retrospective in Nature and derived from population-based studies with several key variables missing
- Unbalanced patient populations with different approaches to account for these differences
- Several unknown confounders with intrinsic selection biases
- Often comparing non-optimal treatments (historical patient cohort)
- Randomized clinical trials in this setting are the only answer
Presented by: Alberto Briganti, MD, PhD, Professor of Urology, Department of Urology, Università Vita-Salute San Raffaele, Milan, Italy
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference, Lugano, Switzerland, April 25th - April 27th, 2024
References:- Stabile A, Pellegrino A, Mazzone E, et al. Can Negative Prostate-Specific Membrane Antigen Positron Emission Tomography/Computed Tomography Avoid the Need for Pelvic Lymph Node Dissection in Newly Diagnosed Prostate Cancer Patients? A Systematic Review and Meta-analysis with Backup Histology as Reference Standard. Eur Urol Oncol. 2022;5(1): 1-17.
- Touier KA, Sjoberg DD, Benfante N, et al. Limited versus Extended Pelvic Lymph Node Dissection for Prostate Cancer: A Randomized Clinical Trial. Eur Urol Oncol. 2021;4(4): 532-539.
- Eastham JA, Heller G, Halabi S, et al. Cancer and Leukemia Group B 90203 (Alliance): Radical Prostatectomy With or Without Neoadjuvant Chemohormonal Therapy in Localized, High-Risk Prostate Cancer. J Clin Oncol. 2020;38(26): 3042-50.
Related Content:


