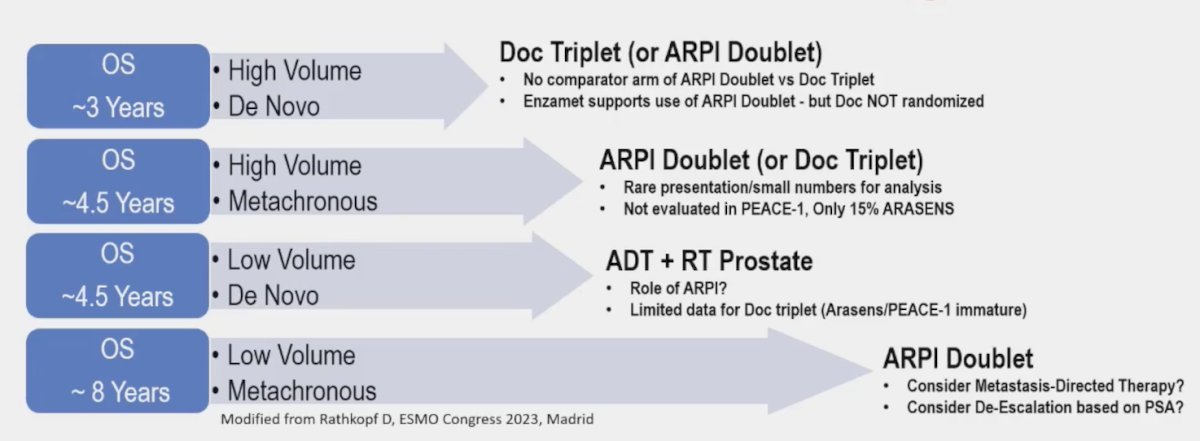
(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on the management of mHSPC, and a presentation by Dr. Dana Rathkopf discussing how to manage patients with low-volume on conventional and high-volume on next generation imaging. Dr. Rathkopf notes that clinical risk groups and treatment selection are already complex for mHSPC, so how do we incorporate next generation imaging into the current paradigm? Currently, overall survival ranges from ~3 – 8 years for mHSPC patients depending on disease volume and timing of presentation:
The clinical conundrum of PET imaging for initial staging and treatment of mHSPC has several pros and cons. The pros include:
- Increased accuracy relative to conventional imaging
- Better detecting small lymph nodes and early/lytic bone disease even at low PSAs
- Potential for targeted treatment options based on imaging results
The cons include:
- Indeterminate findings that can delay treatment and cause patient distress
- The importance of PSMA PET-only and conventional imaging metastasis is unclear
- Do PET-directed treatment decisions lead to better clinical outcomes?
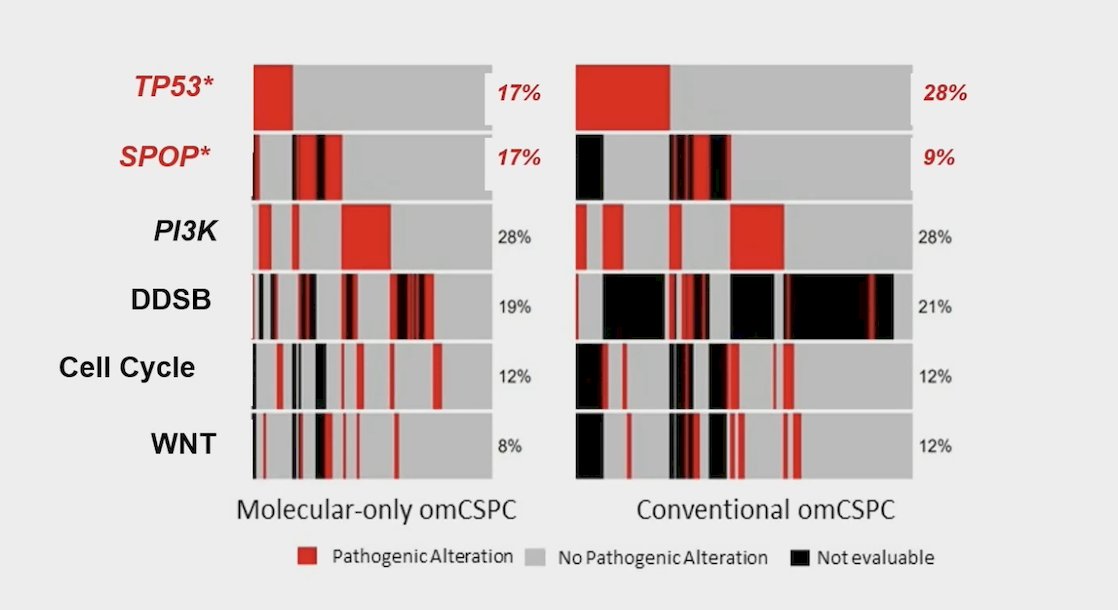
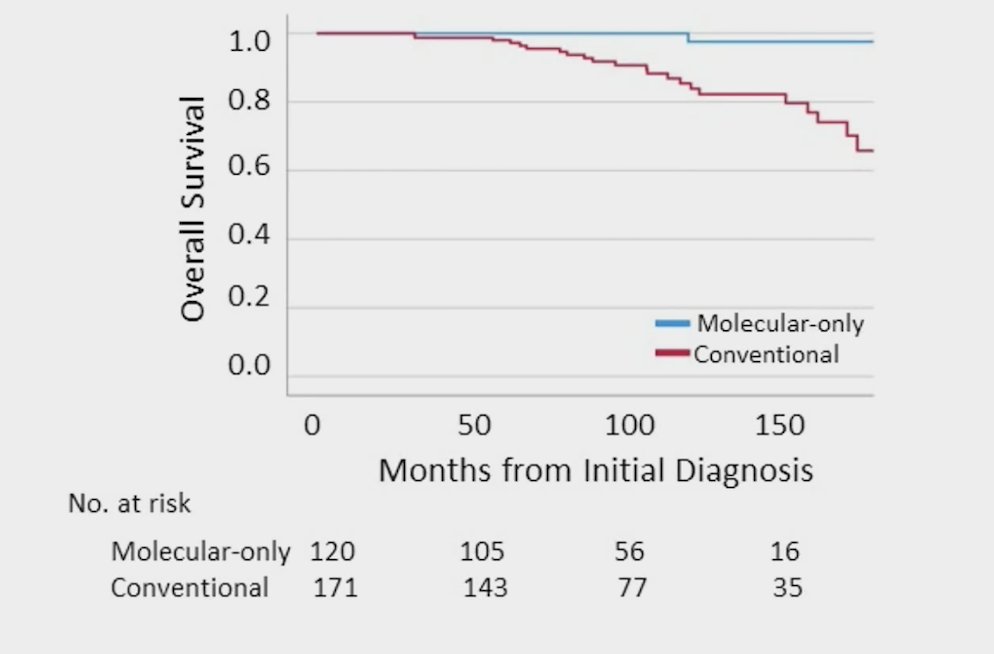
Sutera and colleagues1 recently published an analysis assessing the clinical and genomic differences between advanced molecular imaging detected and conventional imaging detected metachronous oligometastatic castration-sensitive prostate cancer. Among 295 patients included in this study, patients with conventional imaging detected oligometastatic HSPC had significantly higher Gleason grade group (p = 0.032), higher PSA at oligometastatic HSPC diagnosis (8.0 versus 1.7 ng/ml; p < 0.001), and more frequent pathogenic TP53 mutations (28% versus 17%; p = 0.030):
Additionally, patients that had conventional imaging detected oligometastatic HSPC had worse 10 year overall survival (85% versus 100%; p < 0.001):
Dr. Rathkopf wonders if we can extrapolate this concept of PET-only disease being potentially more indolent to polymetastatic mHSPC. Francini et al.2 assessed whether a classification based on time of metastatic disease (after prior local therapy vs de novo) and disease volume (low volume vs high volume) are prognostic for mHSPC patients treated with ADT. Among 436 patients treated at the Dana Farber Cancer Institute included in the analysis, the median overall survival for patients after prior local therapy/low volume disease was 92.4 (95% CI: 80.4-127.2) months and 43.2 (95% CI: 37.2-56.4) months for de novo/high volume disease, whereas intermediate values were observed for after prior local therapy/high volume disease and de novo/low volume disease. A robust gradient for both outcomes was observed (Trend test p < 0.0001) in the four groups:

Data presented at GU ASCO 2024 by Unterrainer et al. suggests that based on conventional imaging, 25.4% of patients have conventional imaging high-volume disease, and 74.6% of patients have conventional imaging low-volume disease. Based on PSMA PET, 40.3% of patients have PSMA high-volume disease 35.8% PSMA low-volume disease, and 23.9% of patients have no PSMA PET positive lesion or only local / N1-disease. Upshift and downshift from conventional imaging to PSMA-PET occur in 40.3% of patients, including 16.4% of patients who are upstaged and 23.9% of patients who are downstaged by PSMA PET:
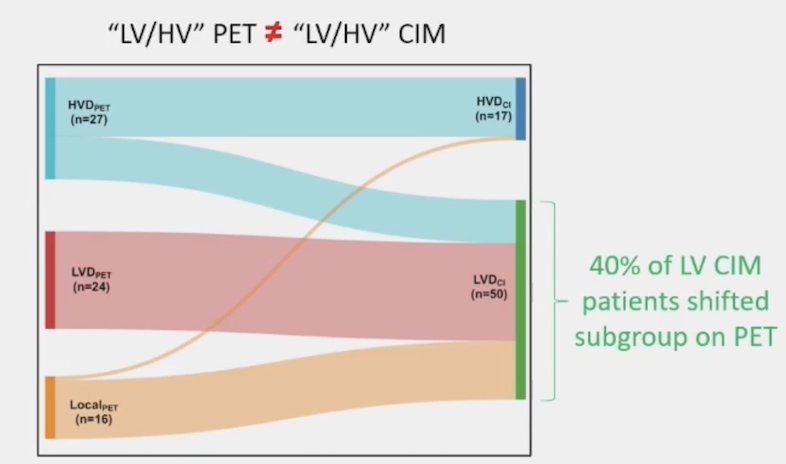
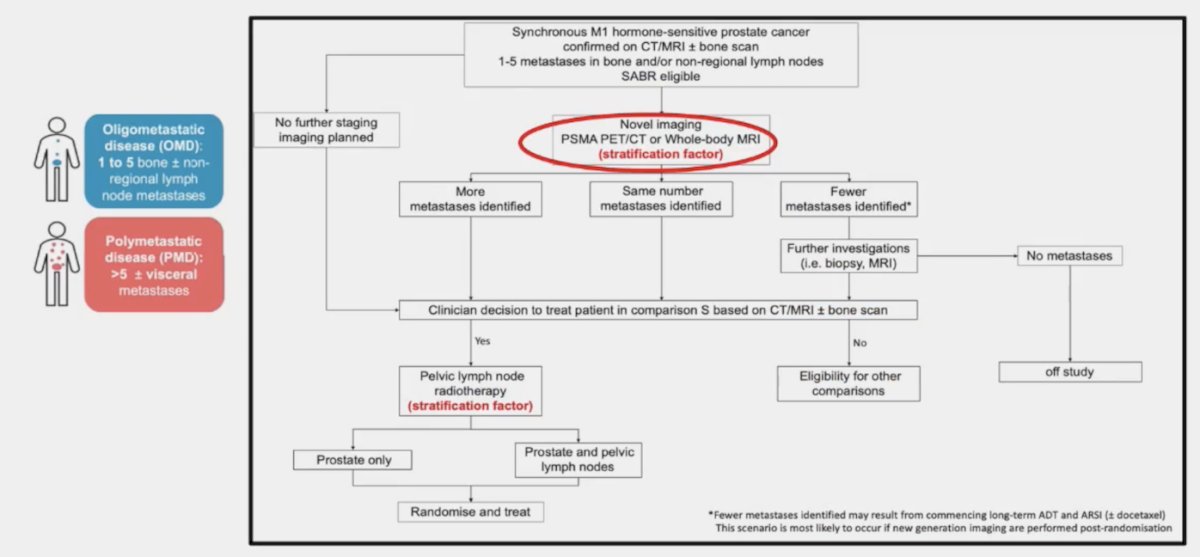
As such, Dr. Rathkopf states that we should use caution when trying to retrofit PSMA PET findings into conventional imaging defined volume subgroups. Dr. Rathkopf then discussed the new STAMPEDE2 trial design (Arm S), which incorporates PSMA PET/CT as a stratification factor and using the more appropriate terminology of “oligometastatic disease” (1-5 bone +/- non-regional lymph node metastases) versus “polymetastatic disease” (>5 bone +/- visceral metastases):
There is increased use of PSMA PET/CT in mHSPC based on accuracy but with limited outcome data. However, there is clinical guidance from several key governing bodies:
- APCCC 2022: For patients with low volume conventional imaging/high volume next-generation imaging, 53% of panelists voted to treat as low volume and 47% voted to treat as high volume
- EAU Annual Congress, Milan 2023 (EAU-EANM-ESTRO-ESUR-ISUP-SIOG): Treatment should not be changed based on PSMA PET/CT findings, in view of the currently available data
- ESMO 2020: Patients with localized prostate cancer according to conventional imaging should not be denied radical local treatment solely because metastatic lesions are identified via next-generation imaging
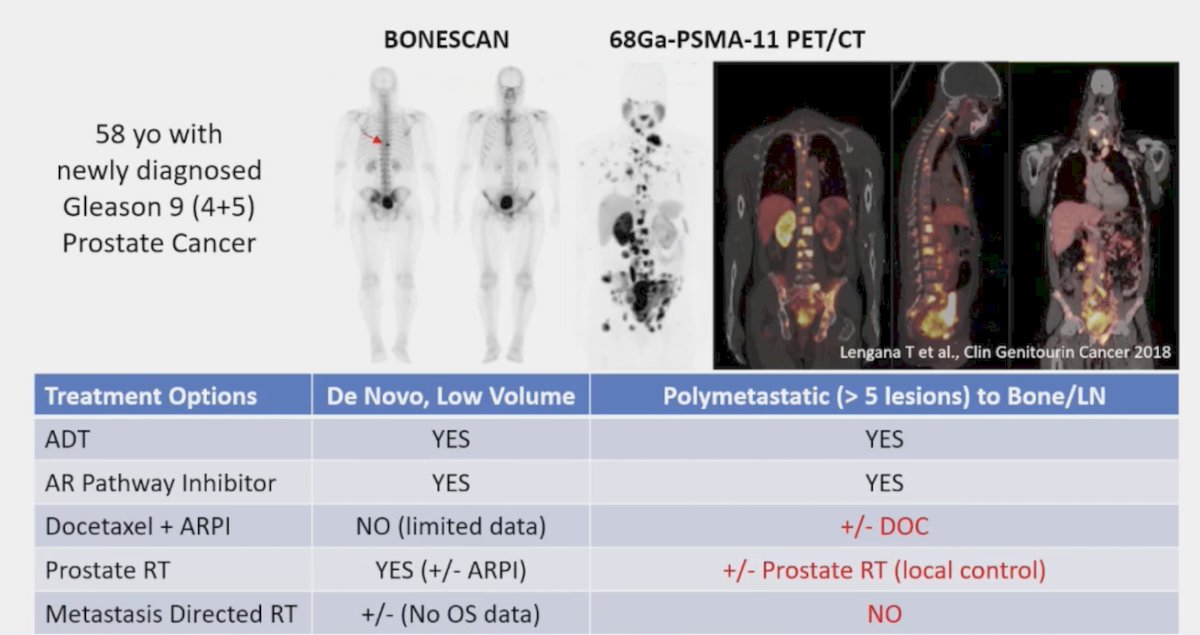
Dr. Rathkopf then discussed a case of a 58-year-old with newly diagnosed Gleason 4+5 prostate cancer whose bone scan showed a solitary vertebral metastases. Given that he is conventional imaging low volume, treatment options include (i) ADT, (ii) ARPI, (iii) prostate radiotherapy (+/- ARPI), and (iv) potentially metastasis directed therapy (although no overall survival data). However, his PSMA PET/CT showed polymetastatic disease, which changes his potential treatment options if we take into consideration the PSMA PET/CT findings:
Dr. Rathkopf provided the following general principles for the treatment of mHSPC in the burgeoning age of next-generation imaging/PSMA PET imaging:
- Clinical subgroups should guide (not decide) treatment decisions
- Conventional imaging volume-based treatment decisions should not be directly extrapolated to PET findings, especially when they are discordant
- PSMA PET imaging is just one piece of the treatment puzzle, we should use caution, as sometimes what you see is not what you get
Dr. Rathkopf concluded her presentation by discussing how to manage patients with low-volume disease on conventional and high-volume disease on next-generation imaging by stating that the metastatic HSPC treatment puzzle has many pieces, and it is our challenge to put them together.
Presented by: Dana Rathkopf, MD, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:
- Sutera P, Song Y, Van der Eecken K, et al. Clinical and Genomic Differences Between Advanced Molecular Imaging-detected and Conventional Imaging-detected Metachronous Oligometastatic castration-sensitive prostate cancer. Eur Urol. 2023 May 10;S0302-2838(23)02790-2.
- Francini E, Gray KP, Xie W, et al. Time of metastatic disease presentation and volume of disease are prognostic for metastatic hormone sensitive prostate cancer (mHPSC). Prostate. 2018 Sep;78(12):889-895.
Related Content:


