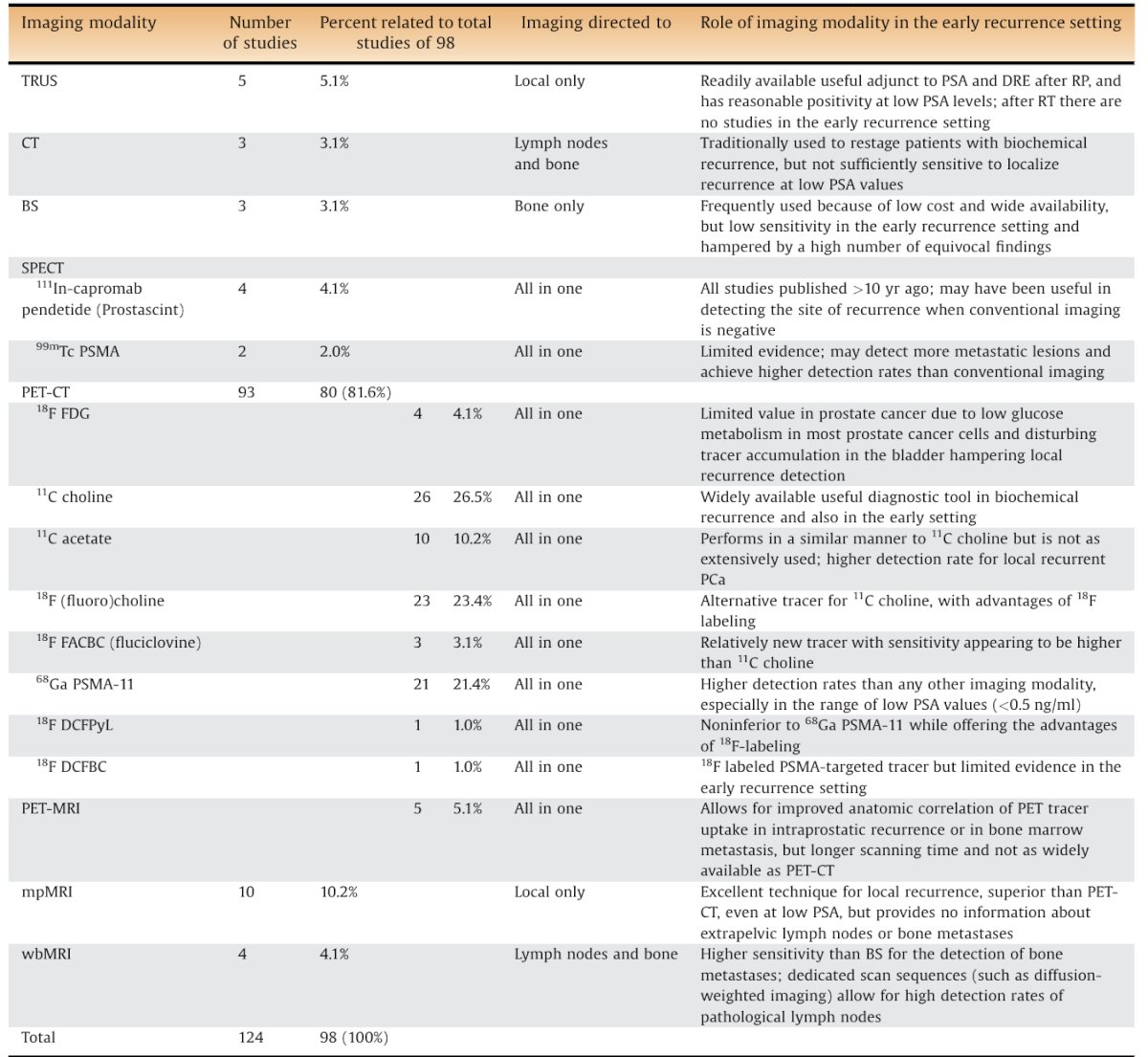
(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on PSMA for diagnostics and treatment, and a presentation by Dr. Stefano Fanti discussing how to utilize the presence or absence of CT findings on a PSMA PET/CT. To start, Dr. Fanti emphasized an important philosophy of science: “If you conclude with A on the basis of good evidence, you cannot use B obtained with less good evidence to confirm A.” Based on multiple studies and reviews, PSMA PET/CT has higher detection rates than any other imaging modality, especially in patients with low PSA values. The following table summarizes the roles of imaging modalities in the setting of early recurrent prostate cancer:1
Thus, as PSMA-PET has higher accuracy (particularly among patients with low PSA levels) than other imaging modalities, we should potentially simply act on the results of the PSMA-PET. However, Dr. Fanti acknowledged that the downfall of this approach, and the “elephant in the room”, is the false positive rate of PSMA-PET.
As part of the Q&A at APCCC 2024, respondents were asked “In the majority of patients with clinically high-risk localized or locally advanced prostate cancer and one PSMA PET positive bone lesions, without a correlate on the CT component of the initial PSMA PET, what do you recommend as the next investigation?” Dr. Fanti was shocked that the most common answer (55%) was correlate with conventional imaging (ie. MRI, x-rays, or bone scintigraphy), with an additional 20% suggesting they would biopsy if feasible, and only 13% reporting they would do no further investigation and treat as M0 disease.
What do we do when we are staging a high-risk patient and there is a positive rib lesion? Dr. Fanti highlighted, in particular, that 18F-PSMA-1007 has nonspecific uptake in bone marrow which may lead to false positive bony lesions:
When this patient above was rescanned with 68Ga-PSMA-11, there was no evidence of a rib lesion:
In 2020, Rauscher and colleagues2 performed a matched-pair comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT to assess the frequency of pitfalls and detection efficacy in biochemical recurrence after radical prostatectomy. Among 204 PSMA PET/CT scans, 18F-PSMA-1007 PET and 68Ga-PSMA-11 PET revealed 369 and 178 PSMA-ligand-positive lesions, respectively. 18F-PSMA-1007 PET revealed approximately 5 times more lesions attributed to a benign origin than 68Ga-PSMA-11 PET (245 versus 52 lesions, respectively):

Another study from Chen et al.3 assessed solitary rib lesions showing PSMA uptake in pre-treatment staging 68Ga-PSMA-11 PET scans. Among 62 men with PSMA uptake in a solitary rib lesion, 54 went on to have a radical prostatectomy and eight underwent radiotherapy. In all, 61 men (98.4%) met the criteria for a benign rib lesion, and only one man had a false-negative malignant lesion. Of the benign rib lesions, there were four false positives reported as possible metastases. Three had percutaneous rib biopsies, two of which came back with benign histology and one was indeterminate. Dr. Fanti noted that these results indicate that the vast majority of these lesions have low-intensity uptake and are benign. He also strongly urged that we should not call faint PSMA uptake as M+ and that requiring a CT scan todeciden on M1 vs M0 is not logical.
There are several open questions that need to be addressed:
- What is the best consensus for PSMA PET reporting?
- What is the impact of imaging on patient management?
- How do we establish cross-specialty interaction?
- How do we handle the use of imaging (PET/CT/MRI) and biomarkers?
Dr. Fanti also acknowledges several major problems that still exist:
- Diagnosis is getting more complex with imaging and blood biomarkers
- Understanding the importance of prognostication versus identification
- There are many unsolved challenges in assessing responses to treatment
Dr. Fanti concluded his presentation discussing how to utilize the presence or absence of CT findings on a PSMA PET/CT with the following take-home messages:
- Use the best tracer necessary
- CT confirmation is not useful or necessary
- Discussions at multidisciplinary tumor boards are necessary
- We should not call faint uptake as M+
Dr. Fanti also mentioned to save the date for February 27-28, 2025 for the first APCCC Diagnostics meeting in Lugano, Switzerland.
Presented by: Stefano Fanti, MD, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:
- De Visschere PJL, Standaert C, Futterer JJ, et al. A systematic review on the role of imaging in early recurrent prostate cancer. Eur Urol Oncol. 2019 Feb;2(1):47-76.
- Rauscher I, Kronke M, Konig M, Matched-Pair Comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT: Frequency of Pitfalls and Detection Efficacy in Biochemical Recurrence after Radical Prostatectomy. J Nucl Med. 2020 Jan;61(1):51-57.
- Chen MY, Franklin A, Yaxley J, et al. Solitary rib lesions showing prostate-specific membrane antigen (PSMA) uptake in pre-treatment staging 68Ga-PSMA-11 positron emission tomography scans for men with prostate cancer: benign or malignant? BJU Int. 2020 Sep;126(3):396-401.
Related Content:


