(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on global access to advanced prostate cancer in low- and lower-middle-income countries, and a presentation by Dr. Vedang Murthy discussing what we can learn from the Indian healthcare system regarding dealing with inequality. The reality of inequality is that the haves and the have-nots will always coexist, so the question is what are we going to do about it?
The Indian healthcare system is a diverse and complex four-tiered network of public and private hospitals that cater to India’s 1.4 billion inhabitants. Roughly 1/4 of patients are insured and 3/4 are uninsured. In India, Dr. Murthy states that it is important to point out that doctors make (and are even expected to make) major treatment decisions for patients. Shared decision-making is less common, as the doctor is expected to know what to do and then tell the patient. A key mantra in Indian healthcare is cost efficiency, to simplify, replace, reduce, and indigenize healthcare. Several examples for each initiative are as follows: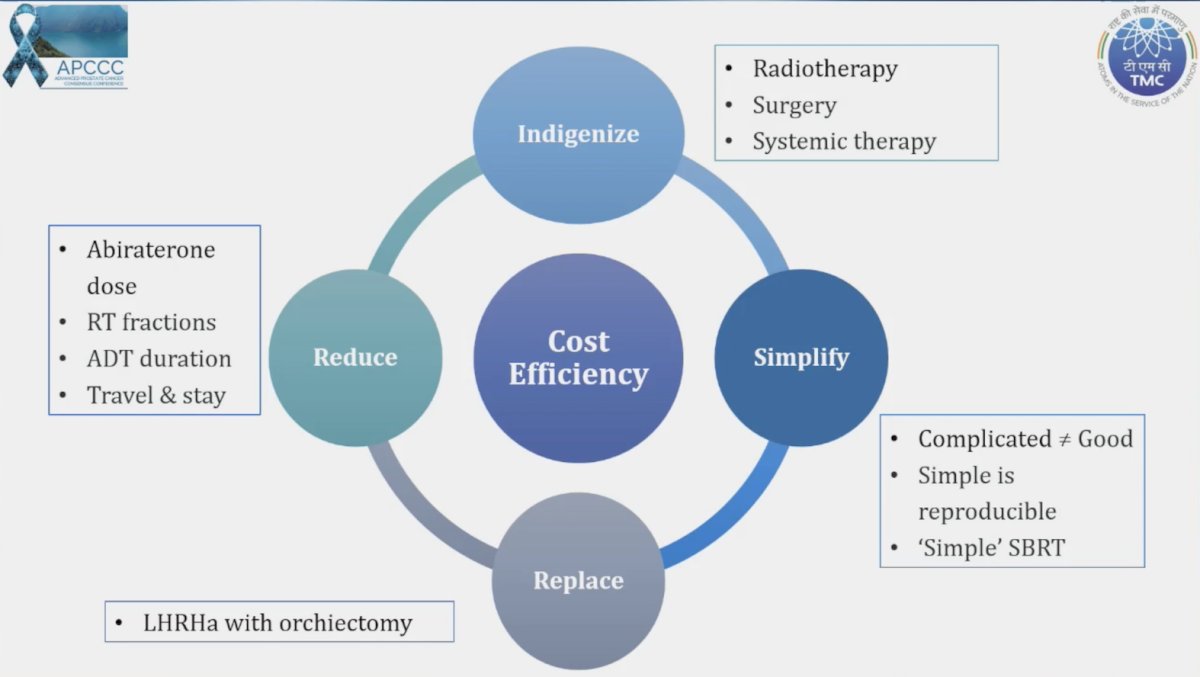
Indigenizing radiotherapy in India has included using bhabhatron (telecobalt), which is robust, low maintenance, runs on a battery backup, and is excellent for palliation: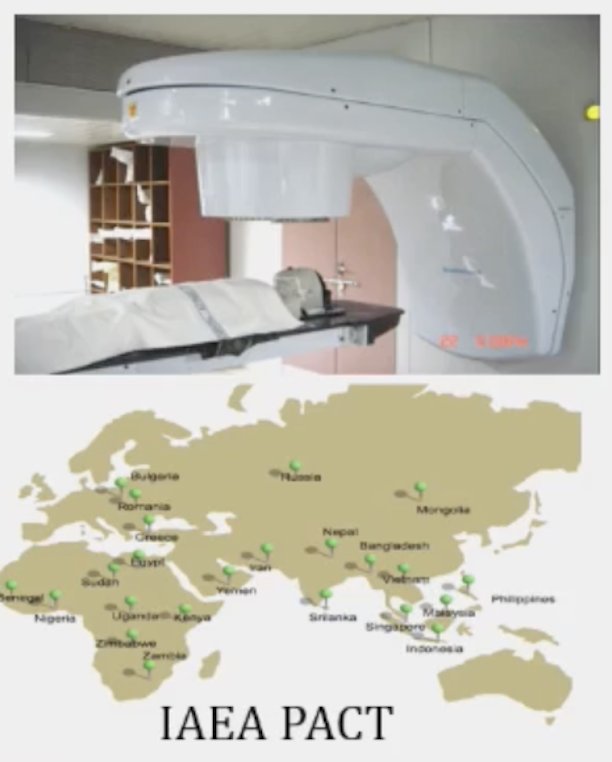
Local solutions for radiotherapy accessories include 3D printing technology, adapting a patient’s anatomy, with an estimated cost of $50 USD (5-10% of the original), thus it is cheap and very effective:
Indigenizing surgery has included utilization of the SSI Mantra robotic platform, which when assessing cost over 300 procedures, is much cheaper than the Da Vinci platform:
Indigenizing systemic therapy includes utilization of primarily generic medications in India. This includes a multistep framework, including a checklist for the manufacturer in order to assess the robustness of the company, a checklist for the drug in order to provide a technical assessment of the drug, and a financial analysis in order to compare top choices, allowing the top 2-3 medications to be sent to pharmacy. One example of a cost-saving choice for systemic therapy is low-dose (250 mg/day) abiraterone with food as an alternative treatment option to full-dose abiraterone (1,000 mg/day). In a study from Patel et al.,1 they assessed a model to estimate the potential financial benefits to individual patients and to estimate overall costs of health care in India if low-dose abiraterone is prescribed. Among 118 respondents, 25% were not aware of the NCCN recommendation to use low-dose abiraterone, 55% were already prescribing it when resources were limited, 7% had already changed their practice, and 29% agreed to switch to a universal practice of using low-dose abiraterone with food. There were 9% of practitioners that would not use low-dose abiraterone. Further, the estimated mean per patient savings was US $3,640, with annual savings of US $182 million in India.
Another hurdle for healthcare in India is to reduce time travel and utilizing the TMC hub and spoke model. The main center (hub) is a large city, such as Mumbai. The hub is responsible for administrative, financial, infrastructural, and educational support. Smaller centers (spokes) are located in 2 tier cities and are technologically linked to the hub. Importantly, the spokes are expected to become hubs over time.
Reduction and simplification include not using traditional stereotactic body radiotherapy (positioning equipment, fiducials, spacer, balloon, MR linac, gating, and transducers), but rather using “simple SBRT” with free simulation, planning, and delivery: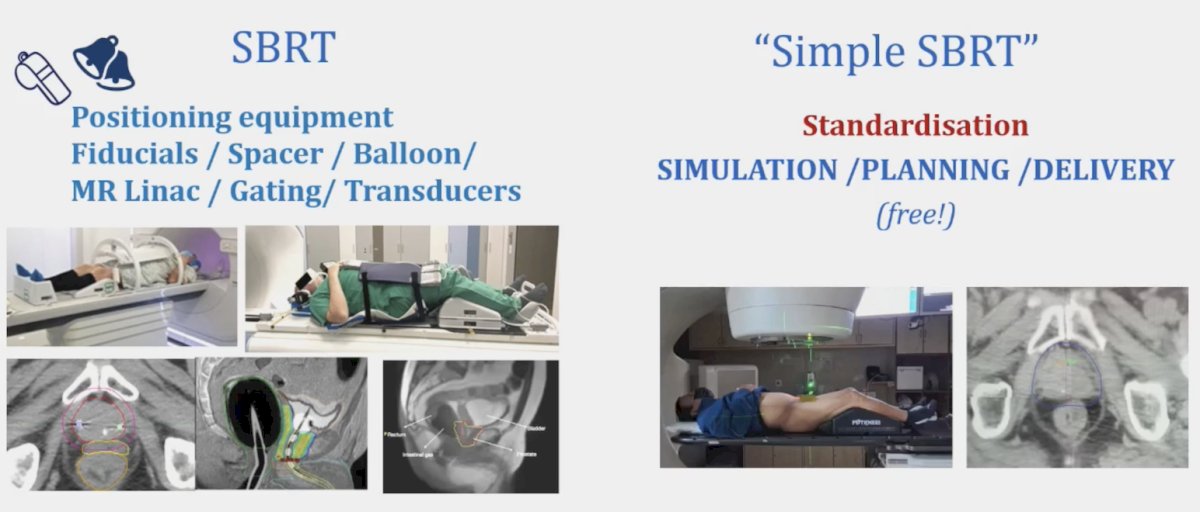
At ESTRO 2023, Dr. Murthy presented an interim analysis of prostate radiotherapy in high-risk or N+ moderate versus extreme hypofractionation (PRIME), noting comparable Grade 3+ GU and GI toxic effects: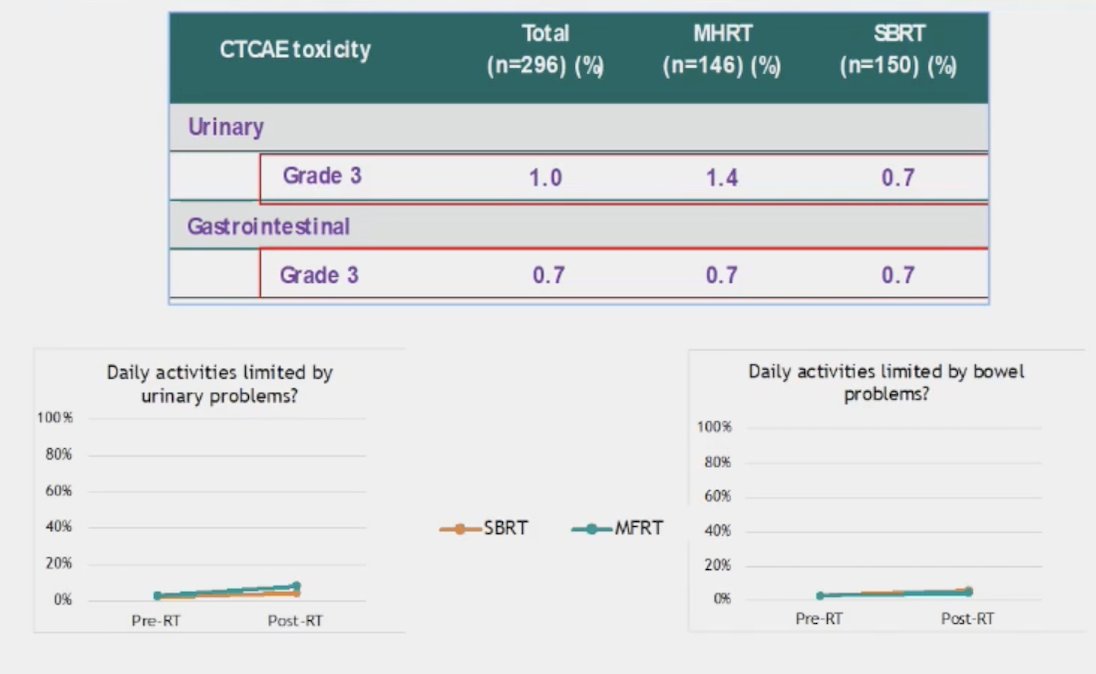
Another important aspect of advanced prostate cancer care is replacing ADT with orchiectomy for M+ disease, saving money on the ADT, and using those cost savings to spend money on life-prolonging therapy, such as ARTAs. In a poll on social media of Indian urologic oncologists, ~50% of respondents felt that if offered an orchiectomy, patients would agree to the procedure. Follow-up visits are less reliable and costly, including additional investigations, salvage treatment, out-of-pocket expenses, and exhaustion of insurance policies.
Dr. Murthy concluded his presentation discussing what we can learn from the Indian healthcare system regarding dealing with inequality by using the Indian word jugaad “A flexible approach to problem-solving that uses limited resources in an innovative way.”
Presented by: Professor Vedang Murthy, MD, DNB, DipEPP, Tata Memorial Centre, Mumbai, India
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:
Related Content:


