(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) held in Lugano, Switzerland between April 25th and 27th was host to a session addressing the management of metastatic hormone-sensitive prostate cancer (mHSPC). Dr. Michael Morris discussed the ‘ideal’ monitoring of mHSPC patients in daily clinical practice.
Conventional imaging in mHSPC remains insensitive to either disease response or progression when compared to PSA kinetics. Additionally, conventional imaging does not image the tumor directly, except for nodes and viscera. A flare phenomenon occurs in up to 50% of patients and confounds interpretation misleading the clinician. As such the Prostate Cancer Working Group (PCWG) 2 and 3 consensuses recommend ignoring the initial on-treatment scan.
The NCCN guidelines currently recommend periodic imaging to monitor treatment response for mHSPC patients.
The treatment landscape for mHSPC has significantly evolved over the last decade, and, as such, Dr. Morris argued that the follow-up method must evolve as well.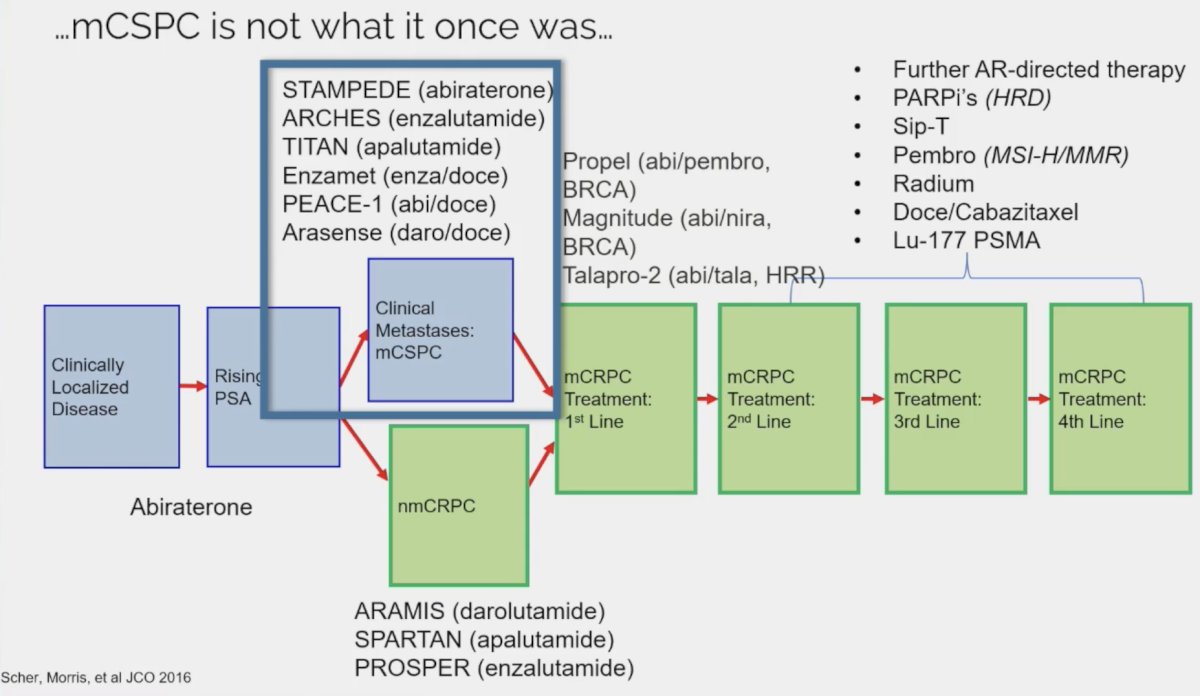
With these changes in the treatment paradigm, we are now observing different patterns of disease progression. Radiographic progression can occur in the absence of PSA progression. A post hoc analysis of the ARCHES trial of enzalutamide doublet therapy in mHSPC patients demonstrated that of 79 patients treated with this doublet combination, 27 (34.2%) developed radiographic progression in the absence of a PSA rise. Conversely, only 28/188 (14.9%) patients in the placebo + ADT arm experienced such an outcome. Patients with radiographic progression, irrespective of PSA progression, had worse survival outcomes highlighting the prognostic significance of these radiographic findings. The investigators of this study concluded that regular imaging is recommended to detect radiographic progression among patients treated with potent androgen receptor pathway inhibitors, such as enzalutamide + ADT, as serial PSA monitoring alone may not be sufficient to detect radiographic progression in many patients.
Is PSMA PET imaging the answer here? And if so, what are the imaging parameters that are most important for assessing treatment response? For metastatic castrate-resistant prostate cancer patients treated with taxanes (docetaxel and cabazitaxel), Shagera et al. demonstrated that PSMA total tumor volume changes were significantly correlated with survival outcomes.1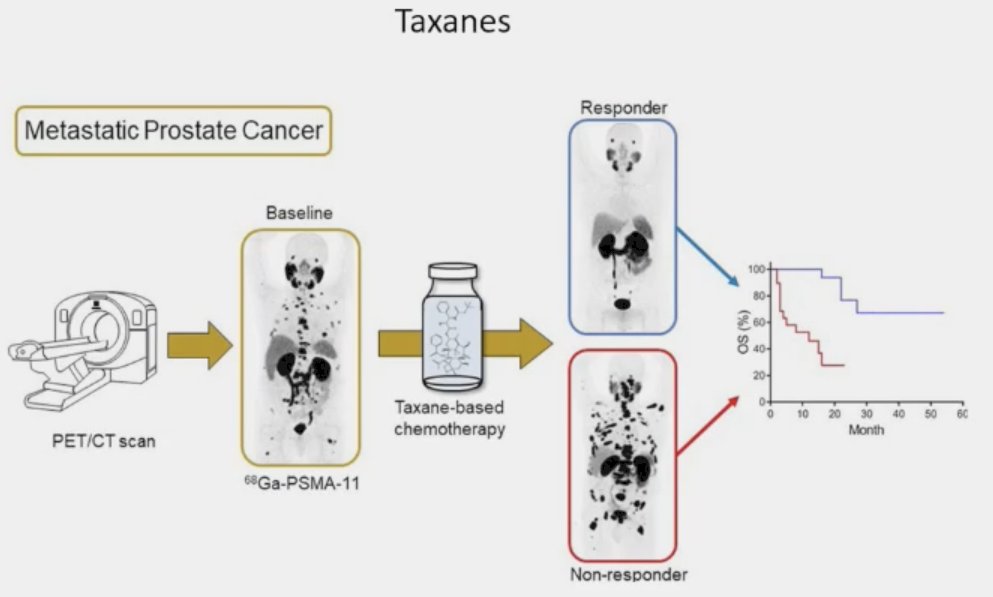
For patients receiving radioligand therapy such as Lu-PSMA, what is the imaging parameter? What is its value compared and combined with other variables such as PSA kinetics and circulating tumor cell count changes?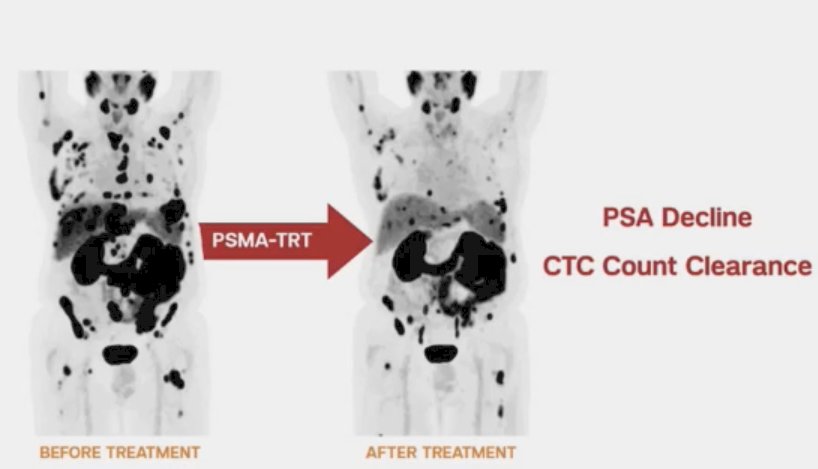
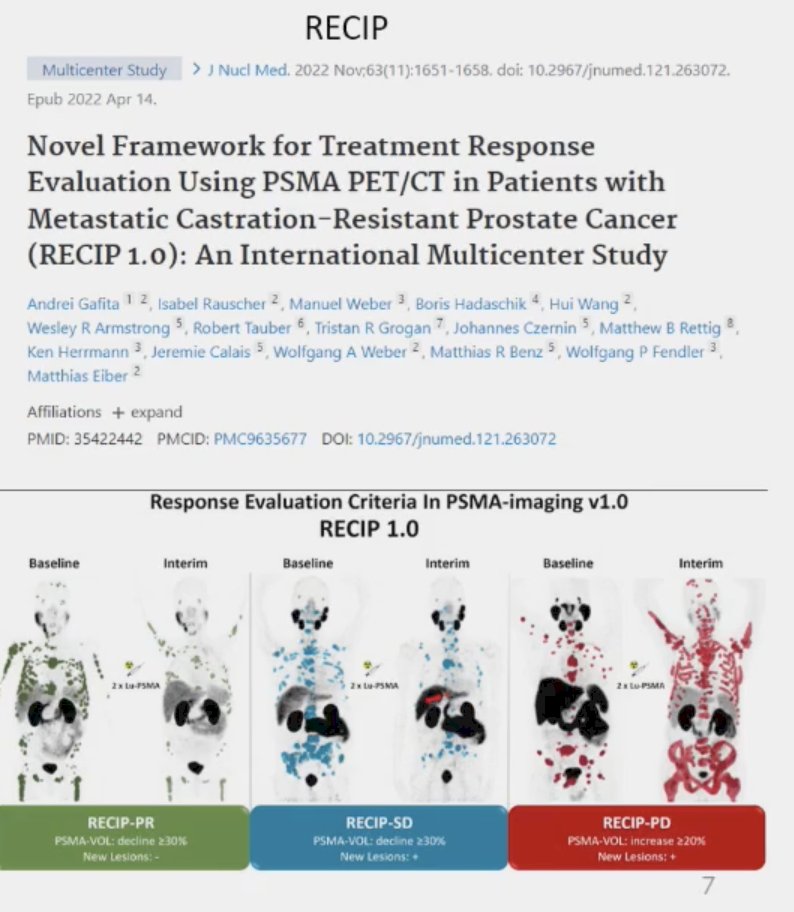
There have been numerous frameworks proposed to assess progression/response criteria, including the PSMA PET Progression (PPP) criteria and Response Evaluation Using PSMA PET/CT in Patients with Metastatic Castration-Resistant Prostate Cancer (RECIP).2,3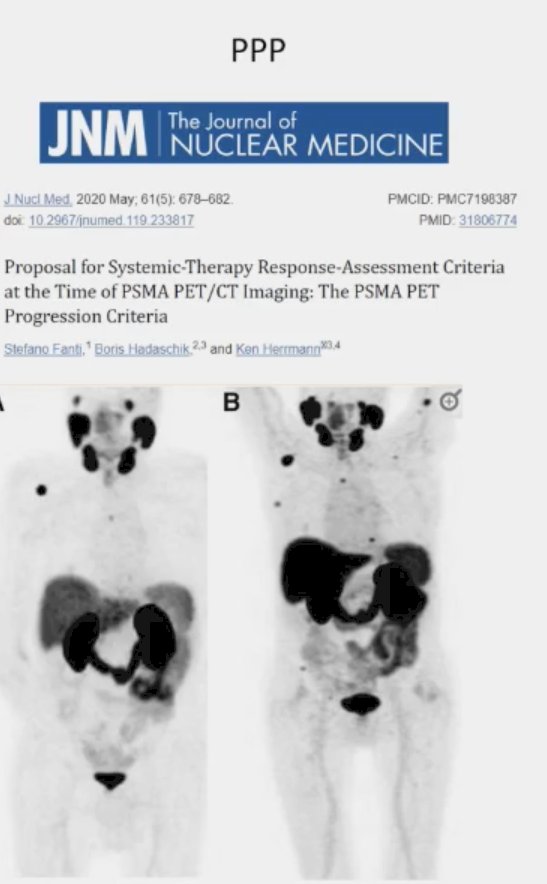
Dr. Morris noted that it is important to be aware of the flare phenomenon on PSMA-PET/CT observed in mHSPC patients treated with androgen receptor inhibitors, owing to the increased expression of PSMA on the cell surface. This variable PSMA expression is more commonly observed in the castrate-sensitive state, relative to the castrate-resistant setting. There is also some early evidence that this flare phenomenon observed after short-term ADT may be an early marker of tumor aggressiveness in treatment-naïve metastatic prostate cancer patients. As the magnitude of the flare phenomenon (i.e., the PSMA ΔSUVmax) increases, the corresponding FDG SUVmax decreases. Additionally, these patients experience worse serum PSA responses with worse flare events.4
He noted the lineage plasticity that occurs in prostate cancer cells, whereby there is a loss of tumor suppressors, activation of oncogenic drivers, and epigenetic changes that occur in ~15% of patients treated with androgen receptor pathway inhibitors. To date, there is no durably effective treatment for these clonal models that rapidly progress and demonstrate heterogeneous biology.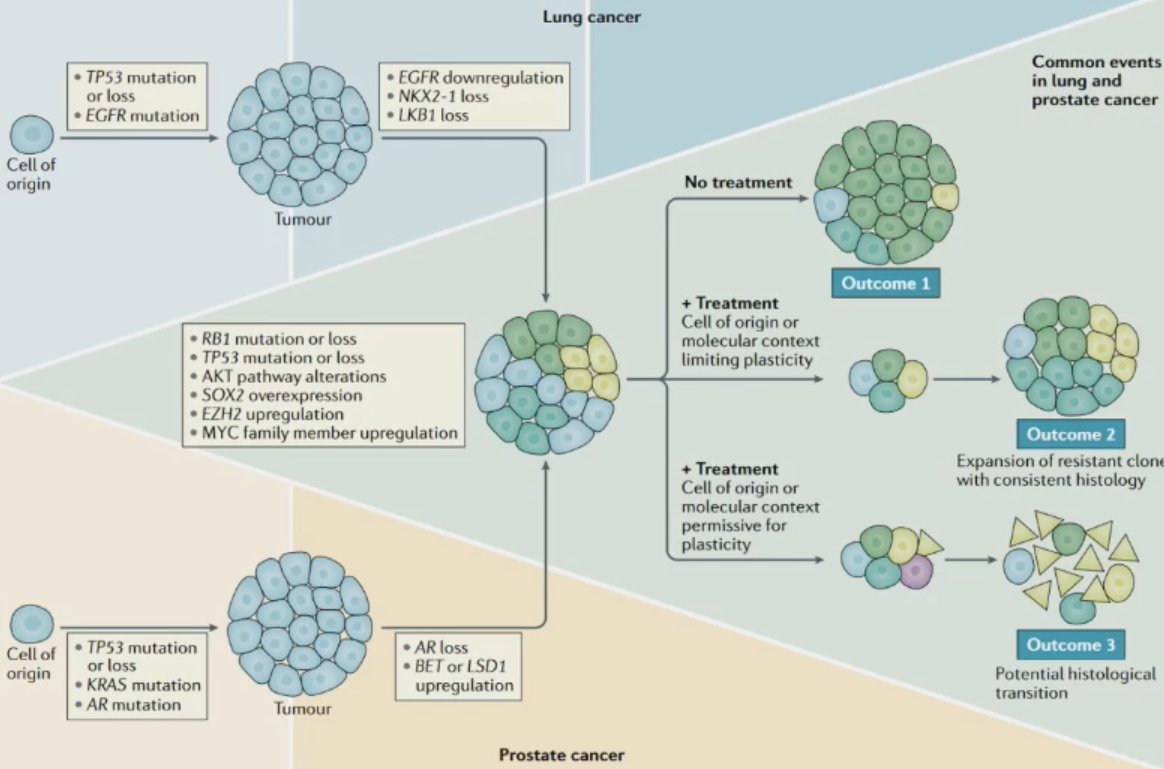
The clonal evolution of these cells leads to a loss of typically expressed cell surface molecules such as PSMA; however, there is an increase in Delta-like ligand 3 (DLL3), which is an actionable target for novel molecular imaging modalities.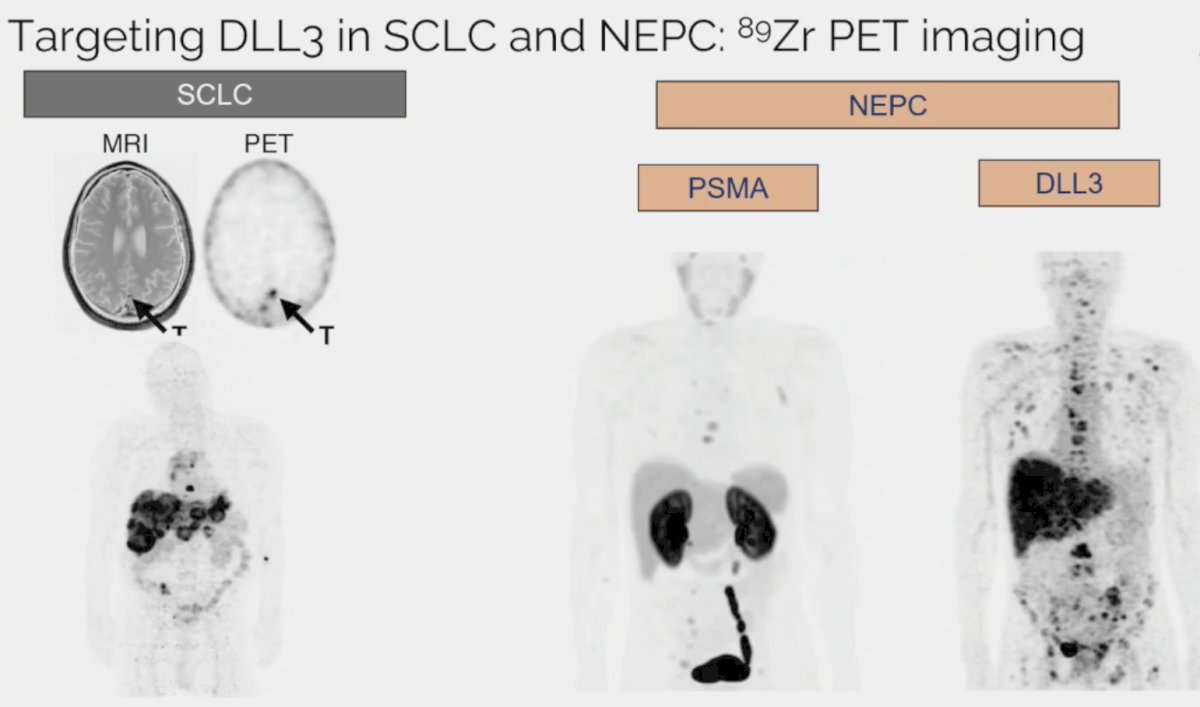
Dr. Morris noted that with regards to PSMA for the imaging of patients with mHSPC, the current guidelines remain inconclusive with regards to their recommendations. The ASCO guidelines note that PSMA may be considered for disease burden determination. The SNMMI recommends considering PSMA if considering metastasis-directed therapy or for assessing disease burden. The NCCN guidelines note that PSMA may be appropriate for staging (+/- conventional imaging techniques).
Dr. Morris concluded his presentation with the following take-home messages:
- Serial imaging should be performed in the contemporary era. Monitoring by PSA alone is insufficient
- Unclear what is the best imaging algorithm (NCCN states 6-12 months)
- PSMA PET imaging does not avoid short-term confounding images
- Generally best not to react to initial scans, just like PCWG4
- May not detect treatment-emergent neuroendocrine prostate cancer
Presented by: Michael Morris, MD, MS, Medical Oncologist, Clinical Director, Genitourinary Medical Oncology Service & Prostate Cancer Section Head, Division of Solid Tumor Oncology, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference, Lugano, Switzerland, April 25th - April 27th, 2024
References:
- Shagera QA, Artigas C, Karfis I, et al. 68Ga-PSMA PET/CT for Response Assessment and Outcome Prediction in Metastatic Prostate Cancer Patients Treated with Taxane-Based Chemotherapy. J Nucl Med. 2022;63(8): 1191-8.
- Fanti S, Hadaschik B, Herrmann K. Proposal of Systemic Therapy Response Assessment Criteria in time of PSMA PET/CT imaging: PSMA PET Progression (PPP). J Nucl Med. 2020;61(5): 678-82.
- Gafita A, Rauscher I, Weber M, et al. Novel Framework for Treatment Response Evaluation Using PSMA PET/CT in Patients with Metastatic Castration-Resistant Prostate Cancer (RECIP 1.0): An International Multicenter Study. J Nucl Med. 2022;63(11): 1651-8.
- Malaspina S, Ettala O, Tolvanen T, et al. Flare on [18F]PSMA-1007 PET/CT after short-term androgen deprivation therapy and its correlation to FDG uptake: possible marker of tumor aggressiveness in treatment-naïve metastatic prostate cancer patients. Eur J Nucl Med Mol Imaging. 2023;50(2): 613-21.
Related Content:


