Patients with aRCC (stage III or IV), unselected for suspicion of an inherited cancer syndrome, were offered germline testing. Germline sequencing was performed as part of MSK-IMPACT, a matched tumor-normal next-generation sequencing platform, that analyzes more 341 cancer associated genes. Of the 341 genes, the authors analyzed 76 genes known to predispose to cancer.
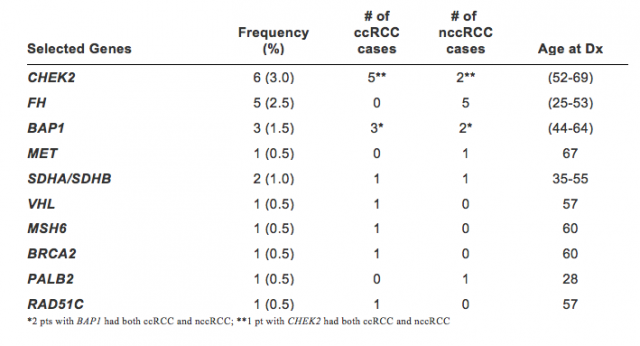
Looking at the results - 203/213 pts accepted testing (median age 55, range 13-55) of whom 73% had clear cell RCC (ccRCC), 92% had metastases, 20% were early onset (≤46 yrs at diagnosis), 9% had a family history of RCC, 6% multifocal RCC at diagnosis, and 15% ≥2 primary malignancies. Pathogenic/likely pathogenic mutations were found in 35 pts (17%): 12 (6%) with mutations in genes associated with familial RCC; and 10 (5%) mutations in high/moderate penetrance genes not linked to RCC (see table below).13 (6%) had mutations in genes of low/uncertain penetrance or for autosomal recessive disease. Mutations were present in 15% of ccRCC and 19% of non-ccRCC. Mutations were not more common in pts with early onset, family history, multifocal RCC, or ≥2 malignancies. Notably, 4/12 pts with mutations in familial RCC genes did not meet the American College of Medical Genetics (ACMG) criteria for testing (1-VHL, 1 – BAP1 1- SDHA, and 1-FH). Additionally, prevalence of CHEK2 mutations was compared to population databases (ExAC) demonstrating that CHEK2 conferred a relative risk of 10.9 (p< 0. 002; 95% CI=3.9-24.7) for RCC.
In conclusion, 17% of aRCC pts had a germline mutation in a cancer-associated gene of which 33% of the high penetrance RCC germline mutations were not identified using standard clinical criteria. Current genetic testing criteria missed 62% of cases, including cases with VHL, BAP1 and FH. This significant finding provides rationale for broad testing. Furthermore, once the increased risk is confirmed, CHEK2 should be included in RCC genetic testing.
Presented By: Maria Isabel Carlo, Memorial Sloan Kettering Cancer Center, New York, NY
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre
Twitter: @GoldbergHanan
at the 2017 ASCO Annual Meeting - June 2 - 6, 2017 – Chicago, Illinois, USA
Reference:
1. Gudbjartsson T, Jonasdottir TJ, Thoroddsen A, et al. A population-based familial aggregation analysis indicates genetic contribution in a majority of renal cell carcinomas. International journal of cancer 2002; 100(4): 476-9.


