Ultimately, a good portion of what she talked about is technical – related to the testing process and the results returned. However, I will highlight some of her important points along the way.
An important early point she made is that the reality on the ground has changed. Whereas in the past, you would assess the patient, order a genetic test for a specific gene if it would affect patient management, and get a single result back, now the paradigm has changed now, we order a genomic test with multiple results first, then assess the patient, and then have to determine what to do with all the results!
Her initial focus was on material already covered by Drs. Cheng and Sartor so I won’t reiterate it here – she highlighted the high rate of somatic and germline mutations in advanced and metastatic prostate cancer patients. She did highlight an emphasis on genetic testing in the Ashkenazi Jewish population as another high risk category – beyond the other indications already mentioned by Dr. Cheng and Sartor.
As Dr. Sartor mentioned, the number of genes recommended for testing by the NCCN seems somewhat limited – BRCA 1, 2, ATM, FANCA, PALB2. Yet, there are so many more mutations in the germline that carry increased PCa risk. Each institution and lab test assesses a different cohort – so know your test! Just because the results don’t mention it doesn’t mean it doesn’t exist!
At Penn, their internal lab has a Penn Consensus panel of common denominators with therapeutic potential (BRCA1, BRCA2, Lynch genes) and “give or takes” (genetic changes for which a clinical trial may or may not become available or genes that may inform relatives)
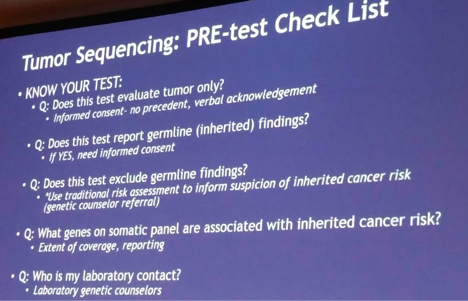
Her next main point: Know your test! This I thought was very interesting and not something many clinicians may be aware of. Each lab runs tests differently. Also genetic testing (of the tumor) may report just somatic mutations, somatic mutations subtracting germline mutations (if additional blood samples or saliva given), or somatic and germline mutations. Understanding the lab and its report is critical to ensure important information isn’t missed.
Somatic only mutations – when a tumor specimen alone is given, all the mutations may be either somatic or germline. You can’t tell unless you send for germline testing
Somatic subtracting germline – you send tumor specimen and blood/saliva. The lab actually removes mutations found in the germline before sending a report. So if the lab sends a report – always check to see if germline mutations were subtracted.
Another important take-home point: If you have any questions about the results being returned or how the lab runs their test, talk to the lab liaison or contact! All CLIA-CAP certified labs have excellent lab liaisons who can answer most questions.
For mutations listed as uncertain clinical significance on reports, you can also go to ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) and enter the mutation. It will give you insight into what other labs (including labs you know and trust) consider this mutation to be benign or pathologic.
Germline:somatic mutation ratio – a general ratio per gene which helps indicate how likely a somatic mutation is due to a germline mutation and warrants germline testing.
DNA repair gene mutations have a high ratio – and usually warrant testing
I thought this was an important slide prior to ordering a genetic test:
However, personal and family history are always important – somatic genetic testing is not the gold standard for hereditary risk assessment and testing.
Post-testing, some questions that should be asked and answered:
1) Has the laboratory provided “variant” interpretation?
For mutations listed as variants of uncertain clinical significance on reports, you can also go to ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) and enter the mutation. It will give you insight into what other labs (including labs you know and trust) consider this mutation to be benign or pathologic.
2) Is this gene associated with a known hereditary cancer susceptibility?
- Some are sure bets and warrant germline testing – ie BRCA1 and 2
- Patients with a somatic mutation and clinical presentation c/w germline mutation should get tested (ie patient with RB1 mutation and prior history of retinoblastoma)
- Genes with moderate penetrance – no guidelines, but strongly encouraged
- Mismatch repair genes – no guidelines, but strongly encouraged
3) Is the gene a common variant of a founder mutation? She listed a few examples, the most common being those found in the Ashkenazi Jewish population.
4) Is this gene commonly mutated in development of this cancer type?
- High germline:somatic ratio – strong recommend germline testing
- Low germline:somatic ratio – no guidelines, but does not appear warranted
Lastly, she highlighted the importance of working with a CLIA-CAP certified lab for the following reasons:

This was a very practical talk for clinicians and gave insight into a side of genetic testing we don’t often see!
Presented by: Jacquelyn Powers, MD
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 2018 ASCO Annual Meeting - June 1-5, 2018 – Chicago, IL USA


