Dr. Spratt later spoke in favor on the role of prognostic biomarkers in determining a patient’s risk of recurrence, irrespective of the treatment type he had received. It has been demonstrated that pre-salvage radiotherapy PSA is one of the most important variables. The higher the PSA, the worse of the distant metastasis free survival (Figure 1).
 PSA levels correlated to distant metastasis free survival
PSA levels correlated to distant metastasis free survivalPost salvage radiotherapy PSA is correlated positively to the detection rate of a PET choline scan. The higher the PSA, the more lesions are diagnosed in the PET choline scan. Unfortunately, the rate of early salvage radiotherapy for recurrent PC (PSA<0.5 ng/ml) is under-utilized with only 1/6 men end up receiving it (Figure 2).
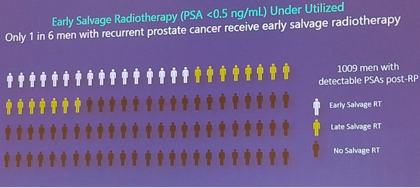 Early salvage radiotherapy rates
Early salvage radiotherapy ratesAccording to the NCCN guidelines, genomic classifiers such as the Decipher test can help personalize risk. A low Decipher score, even with a Gleason score of 8 (4+4) in the final radical prostatectomy specimen pathology, tells us the risk of metastasis is very low. In contrast, a high Decipher score in patients with a lower Gleason score, can mean a substantial risk for metastasis further down the line.
Predictive biomarkers can help determine a patient’s risk of recurrence, specific to the treatment type he received. There are no prospectively validated predictive biomarker to guide radiotherapy, or the use of hormonal therapy with radiotherapy. The PAM50 – basal/luminal subtyping for PC has shown that for Luminal B type, ADT confers a significant benefit in distant metastasis free survival, while this advantage is not shown in the basal subtype.
Unfortunately, there is no level 1 evidence to show an advantage of adjuvant vs. early salvage radiotherapy. Data has shown that hormonal therapy should not be used for men with low PSA levels prior to salvage radiotherapy. Salvage radiotherapy and hormonal therapy should be given only to men with “late” salvage radiotherapy and a PSA > =0.7 ng/ml. ADT alone treatment is not curative, although it prolongs life. The ideal population for this treatment type is unclear, and should probably include patients with a contraindication to radiotherapy. It may also be beneficial for patients with significant extra-pelvic disease.
Dr. Spratt then discussed his own currently recruiting study (NRG GU-006) comparing post-surgery patients with BCR, that are randomized to receive external beam radiotherapy plus either placebo or Apalutamide for 6 months (Figure 3).
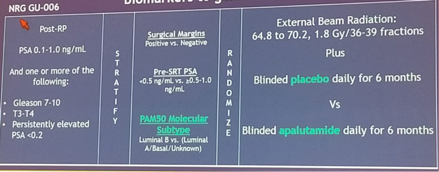 Dr. Spratt’s NRG-GU-006 currently accruing trial
Dr. Spratt’s NRG-GU-006 currently accruing trialIn summary, Dr. Spratt concluded that we should utilize calculated absolute risks using nomograms and genomics. This should include life expectancy and distant metastasis risk. Adjuvant radiotherapy is ideal for patients with >50% risk of recurrence after surgery. Salvage radiotherapy alone is standard of care for men with PSA <=0.5 ng/ml. Salvage radiotherapy with hormonal treatment is standard of care for men with PSA >= 0.7 ng/ml. Future work is needed to understand the role of systemic therapy without postoperative radiotherapy. We are in great need of predictive biomarker trials to guide radiotherapy and hormonal therapy usage.
Presented by: Daniel Spratt, Michigan, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the 2018 ASCO Annual Meeting - June 1-5, 2018 – Chicago, IL USA


