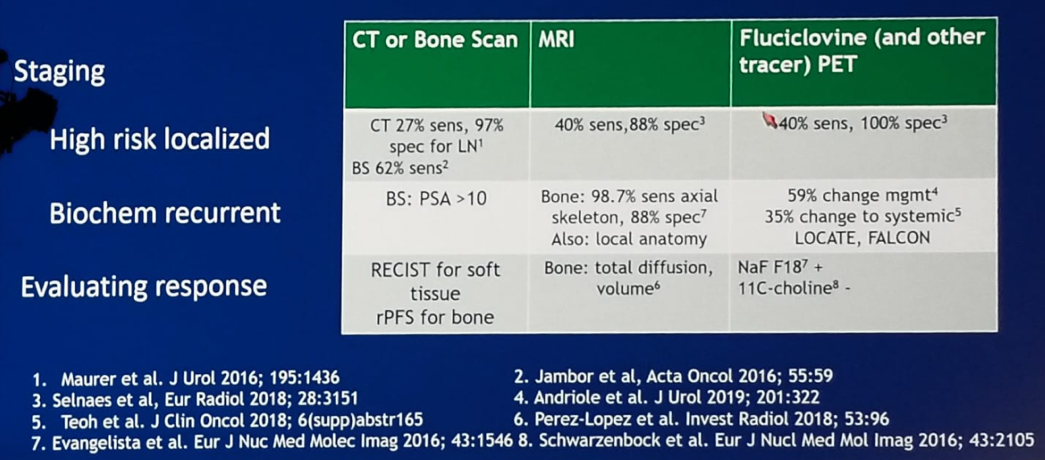
The most commonly used imaging modalities in prostate cancer include computerized tomography or bone scan, magnetic resonance imaging, and fluciclovine (and another tracer) PET scans. These imaging modalities are far from ideal, and there is much to improve, as can be seen in Table 1, with relatively low sensitivity percentages for all modalities.
Table 1 – How well do current imaging modalities perform?
In the setting of high-risk localized prostate cancer, lymph nodes detected by imaging pose a dilemma. It is not clear if we need to remove all of them in the suspicious area or just the ones with the enhanced PET-tracer uptake. Even if we remove all the nodes, we do not have the data showing that it leads to lower recurrence rates, and the associated increased complication rate is also something that needs to be factored in.
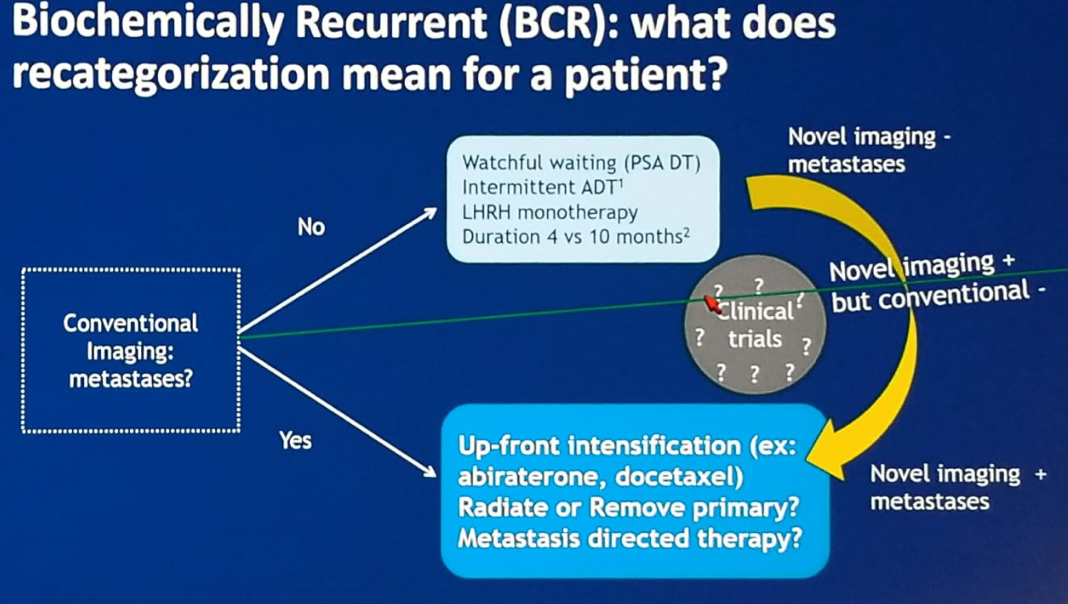
In the setting of biochemical recurrence after primary treatment, we need to understand what the concept of recategorization means for the patient. Using conventional imaging, a patient is categorized to either being treated with watchful waiting, if no metastases are found, or up-front intensification of treatment, if metastases are discovered.1,2 However, with novel imaging, this categorization could potentially be changed (Figure 1), leading to different treatment strategies.
Figure 1 – Categorization of patient according to conventional imaging and change expected with novel imaging:
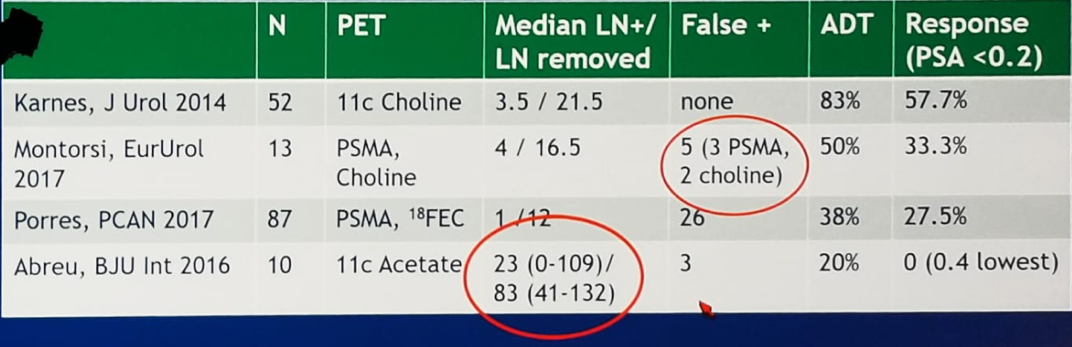
A large study assessed the clinical response of patients following robotic salvage retroperitoneal and pelvic lymph node dissection for “node-only” recurrent prostate cancer (based on positive PET scans).3 The results demonstrated that PSA had decreased in 83% of patients after removal of histologically positive nodes. However, more nodes were histologically positive than were seen on imaging, and lymphedema had occurred more often following surgery. This and other similar studies have shed some light on the sensitivity/specificity of PET imaging, as can be seen in table 2.
PET imaging can be used to assess response, but it is still far from ideal and varies from patient to patient. There are still more questions than answers regarding its role,4 including what is the optimal timing (PSA level) for performing a novel scan in search of micrometastases? Moreover, if novel imaging reveals more diffuse disease, will all patients benefit from adding chemotherapy in the form of the docetaxel?
Table 2 – Studies examining the role of salvage lymph node dissection and its association with the results of PET imaging:
Concluding her talk, Dr. Dorff summarized a few points. Novel imaging can potentially reduce over-treatment (metastasis-directed therapy) and under-treatment (no intensification). It can also accelerate drug development, as PET response parameter that correlates with survival would give an earlier measure of whether treatment is working, compared to the commonly used term of radiographic progression-free survival.
There is still plenty of data that we need to acquire about novel imaging, including comparative sensitivity, accuracy (histologic verification, and response to radiation), and the outcomes of treatment decisions that should be made based on novel imaging (i.e., survival).
Presented by: Tanya B. Dorff, MD, Head of the Genitourinary Cancers Program, Associate Clinical Professor, Department of Medical Oncology & Therapeutics Research, City of Hope, Duarte, California, United States
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2019 ASCO Annual Meeting #ASCO19, May 31-June 4, 2019, Chicago, IL USA
References:
- Crook et al. "Intermittent Androgen Suppression for Rising PSA Level." New England Journal of Medicine. 2012. DOI: 10.1056/NEJMc1211950.
- Klotz et al. " A Phase II, Randomized, Multicenter Study Comparing 10 Months versus 4 Months of Degarelix Therapy in Prolonging the Off Treatment Interval in Men with Localized Prostate Cancer Receiving Intermittent Androgen Deprivation Therapy for Biochemical Recurrence following Radical Local Therapy"J Urol 2018; 200: 335.
- Abreu A. et al. "Robotic salvage retroperitoneal and pelvic lymph node dissection for 'node-only' recurrent prostate cancer: technique and initial series," BJU International Journal. 2017. doi: 10.1111/bju.13741.
- Vapiwala et al. "Strategies for Evaluation of Novel Imaging in Prostate Cancer: Putting the Horse Back Before the Cart." Journal of Clinical Oncology. 2019. doi: 10.1200/JCO.18.01927.


