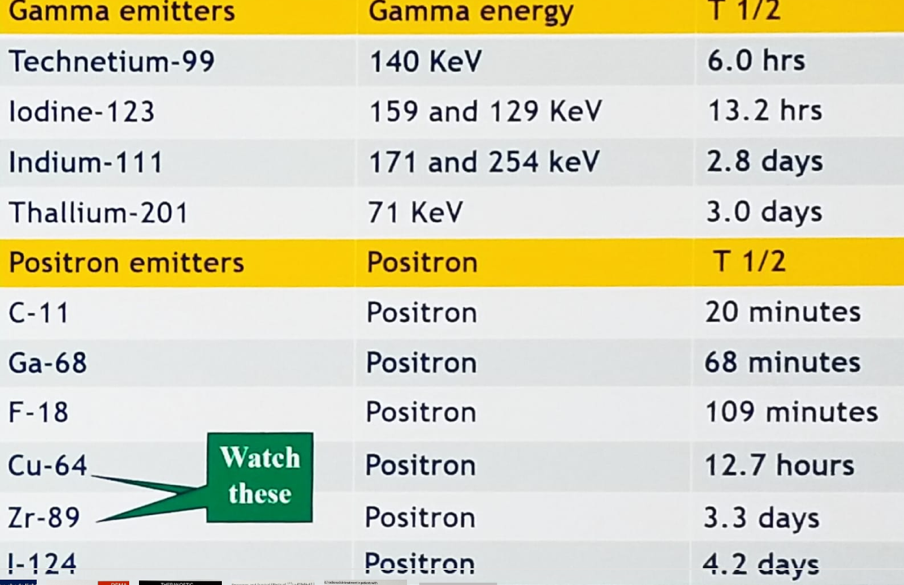
Table 1 – Gamma emitters used in PET imaging:
Many local therapy failures are secondary to a poor understanding of disease localization. Prostate cancer imaging is especially challenging given bone involvement because conventional imaging assesses bone stroma and not the tumor.
The investigation of PET in “localized therapies” is now actively being explored. It is important to acknowledge that PSMA-PET is likely more than ten times better than conventional imaging, but no imaging will ever be perfect. The localization of disease is just the beginning of imaging, and many other factors need to be considered:
- Microenvironment assessment – (Hypoxia, immune infiltrates, and stromal integrins). For example, there has been published data1 on the usage of 89Zr-atezolizumab imaging as a non-invasive approach to assess clinical response to immunotherapy (PD-L1 blockade in cancer), as shown in Figure 1. These data show that clinical responses correlated better with PD-L1 imaging than with immunohistochemistry or RNA sequencing.
- Predictive and prognostic biomarker – Patient selection for treatment
- Linkage to underlying genotype
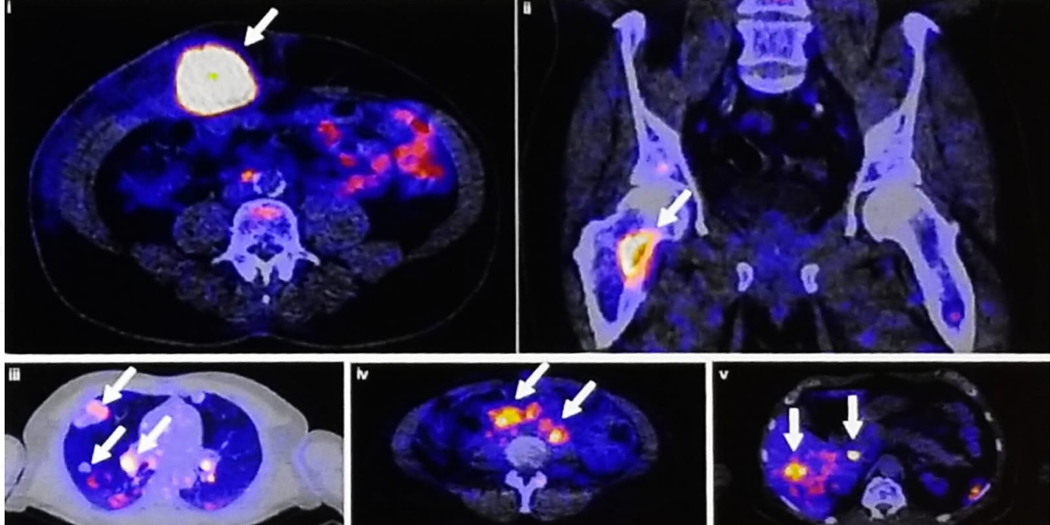
Figure 2 - Rapid PSMA-PET response after initiating androgen deprivation therapy:

Dr. Sartor ended his discussion asking a very important question: While there is no doubt that significant advances have been made in novel PET imaging, enabling us to see the disease better and more of it, does it really matter in the long run? Does it change patient outcomes? Unfortunately, to date, we cannot answer this.
Presented by: A. Oliver Sartor, MD, Professor of Medicine, Medical Director, Tulane Cancer Center, New Orleans, Louisiana
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, @GoldbergHanan at the 2019 ASCO Annual Meeting #ASCO19, May 31- June 4, 2019, Chicago, IL USA
References:
- Bensch F. et al. 89Zr-atezolizumab imaging as a non-invasive approach to assess clinical response to PD-L1 blockade in cancer. Nat Med. 2018 Dec;24(12):1852-1858
- Jadvar H. et al. Prediction of time to hormonal treatment failure in metastatic castrate-sensitive prostate cancer with 18F-FDG PET/CT. J Nucl Med. 2019 Mar 29.
- Fox JJ. et al. Positron Emission Tomography/Computed Tomography-Based Assessments of Androgen Receptor Expression and Glycolytic Activity as a Prognostic Biomarker for Metastatic Castration-Resistant Prostate Cancer. JAMA Oncol. 2018 Feb 1;4(2):217-224.


