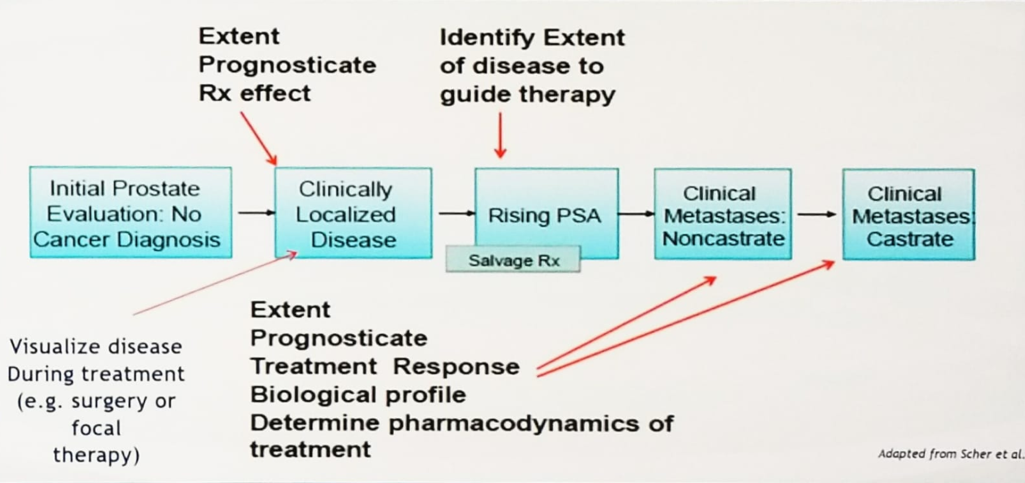
Figure 1 – Role of imaging in the various stages of prostate cancer
The performance of PSMA-PET in biochemical recurrence is correlated to the PSA level. The higher the level of PSA, the higher positivity of the PSMA-PET scan (Figure 2).1 Examining the data from a UCLA-UCSF study,2 the distribution of lesions in men with biochemical recurrence is shown in Figure 3, demonstrating the increased detection rate of PSMA-PET with rising PSA, and showing that most lesions occur in multiple regions and not in the prostate bed (Figure 3).
Figure 2 – Correlation of PSMA-PET positivity to PSA values:
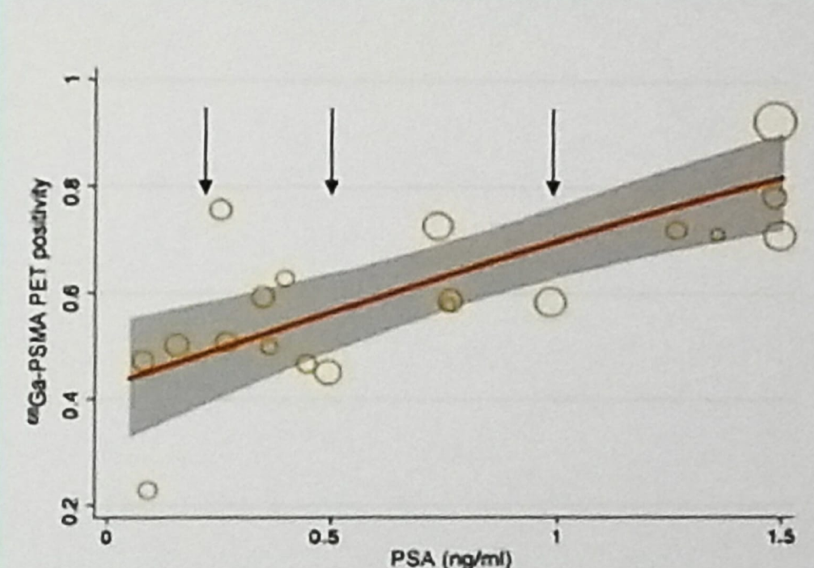
Figure 3 – UCLA-UCSF study showing the distribution of lesion in men with biochemical recurrence:

There is a plethora of data showing that there is between 29% to 76% management change after using PSMA-PET imaging in patients with biochemical recurrence.3-7 These include decreased use of salvage radiotherapy to the prostate bed, increased use of salvage node dissection, stereotactic radiotherapy, and androgen deprivation therapy (ADT).
Usage of PSMA-PET has raised some important questions that need to be answered. These include:
- Whether prostate bed only lesion permit omitting of node-irradiation?
- Does the detection of nodes outside the usual radiation fields lead to enhanced radiation delivery that makes a difference in outcome?
- Does salvage lymphadenectomy or stereotactic body radiation therapy improve meaningful outcomes for regional or oligometastatic disease?
- Should salvage radiation be delayed until there is a detectable disease?
Dr. Reiter concluded his presentation and stated that PSMA-PET is sensitive and specific for local recurrence and regional/distant metastasis in the setting of biochemical recurrence. It is not a perfect imaging test, and still misses many sites, smaller than 5 mm. Its sensitivity is only 30%-40% of high-risk disease. However, it is considerably better than conventional imaging used so far for high-risk disease.
To date, imaging has not changed management, but new technology raises new clinical management dilemmas, and we still need to decipher how PSMA-PET should alter management in specific conditions, and most importantly, whether it improves disease outcomes at all.
Presented by: Robert Evan Reiter, MD, Urology Surgery, Complex General Surgical Oncology, Institute of Urologic Oncology, University of California Los Angeles, Los Angeles, California, United States
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2019 ASCO Annual Meeting #ASCO19, May 31-June 4, 2019, Chicago, IL USA
References:
- Perera et al. "Sensitivity, Specificity, and Predictors of Positive 68Ga-Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer: A Systematic Review and Meta-analysis." European Urology. 2016. doi: 10.1016/j.eururo.2016.06.021.
- Fendler et al. "Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial."JAMA Oncology. 2019. doi:10.1001/jamaoncol.2019.0096.
- Van Leeuwen et al. "(68) Ga-PSMA has a high detection rate of prostate cancer recurrence outside the prostatic fossa in patients being considered for salvage radiation treatment." BJU InternationaI. 2016. doi: 10.1111/bju.13397.
- Calais et al. "Potential impact of 68Ga-PSMA-11 PET/CT on prostate cancer definitive radiation therapy planning." The Journal of Nuclear Medicine. 2018. doi: 10.2967/jnumed.118.209387.
- Han et al. "Impact of 68Ga-PSMA PET on the Management of Patients with Prostate Cancer: A Systematic Review and Meta-analysis." European Urology. 2018. doi: 10.1016/j.eururo.2018.03.030.
- Bianchi et al. BJUI 2018
- Albisinni et al. "Impact of 68Ga-PSMA PET on the Management of Patients with Prostate Cancer: A Systematic Review and Meta-analysis." BJU International. 2018. doi: 10.1016/j.eururo.2018.03.030.


