The incidence of prostate cancer in the US has been decreasing over time, as seen in Figure 1. Additionally, the treatment paradigm in this era of precision medicine has changed significantly, in each disease stage of prostate cancer, with the use of genomics, molecular imaging and clinical trials (Figure 2).
Figure 1 – Incidence of prostate cancer diagnosis and death in the US: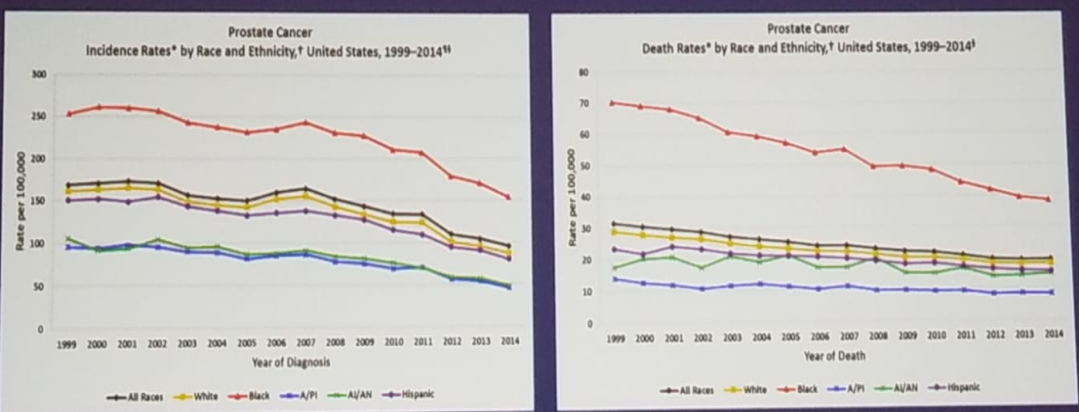 *CDC.GOV
*CDC.GOV
Despite these advances, treatments options are not equal and accessible for all. First, it is important to acknowledge, that there are significant genomic disparities in the different races, as has been published by Spratt D. et al1 (Figure 3). There are also genomic disparities in patients with metastatic prostate cancer. In a multicenter study analyzing men with metastatic prostate cancer, the incidence of germline mutations in genes mediating DNA-repair processes was 11.8%, which was significantly higher than the incidence among men with localized prostate cancer2 (Figure 4).
Figure 2 – Prostate cancer treatment paradigm changes in the era of precision medicine: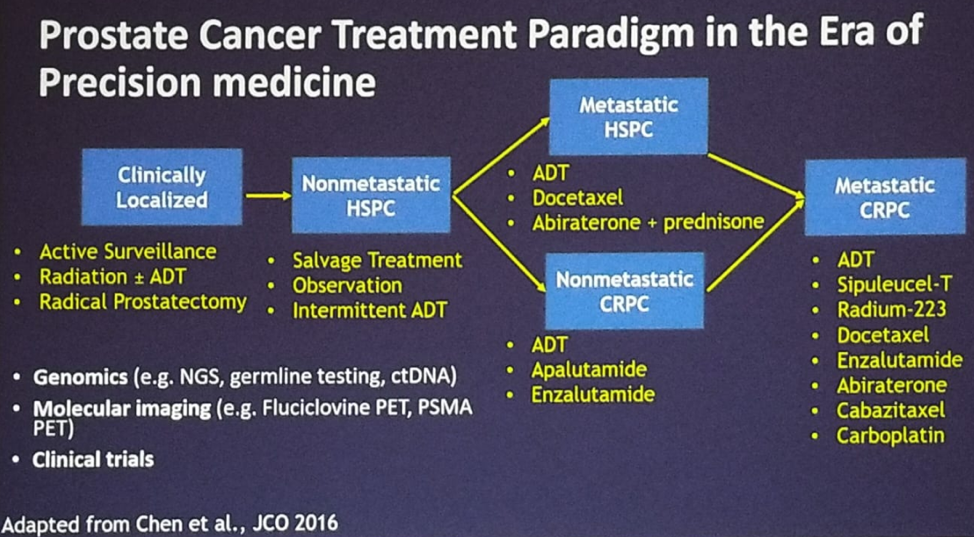
Figure 3 – Genomic disparities in prostate cancer by race: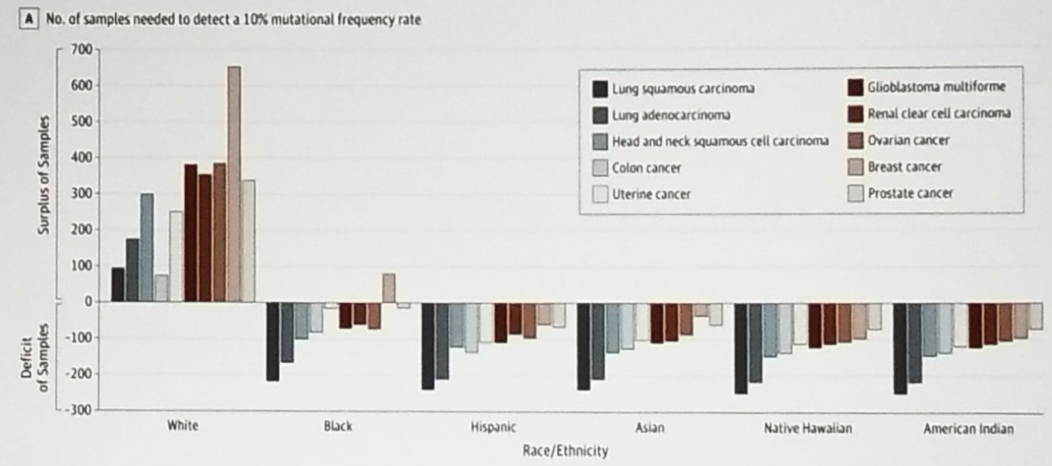 *Spratt D. et al. JAMA ONC 2016
*Spratt D. et al. JAMA ONC 2016
Figure 4 - Genomic disparities in germline mutations in men with metastatic prostate cancer: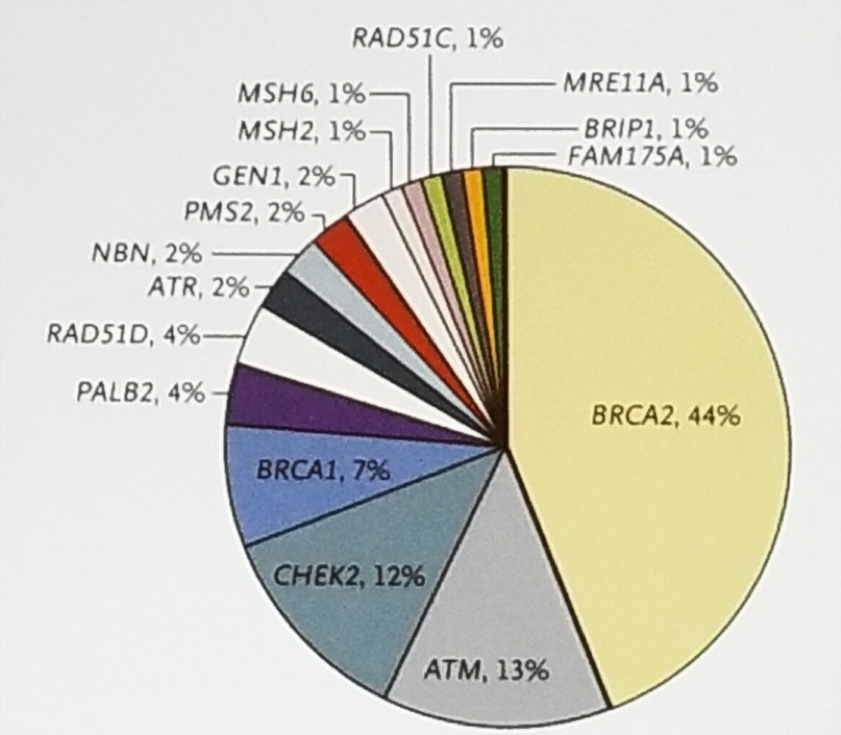 *Pritchard CC et al. NEJM 2016
*Pritchard CC et al. NEJM 2016
There are also molecular imaging disparities with different referral patterns for PET imaging. In a study assessing 82 patients referred for Fluciclovine-PET imaging, 69% were white, and only 11% were black.3 More importantly, when analyzing patients accrued to clinical trials, there are significant race disparities, and a significantly lower percentage of black people are enrolled in these trials (ranging from 2-5.8%, in castrate resistance prostate cancer trials).4,5 This underrepresentation of black people has important implications as black people might not receive the same treatment options as white people.6 From the few studies that have race-specific data in their reporting, there is some evidence to note that black men might have a better response rate to certain treatments compared to white men (Table 1).
Summarizing her talk, Dr. Borno stated that in the era of precision medicine, differential access to emerging technologies will worsen cancer disparities. Non-uniform access to genomic testing and molecular imaging will drive clinical trial disparities. Finally and most importantly, tracking demographics of clinical trial participants is an important barometer in prostate cancer treatment equity.
Table 1 – Race-specific reporting in prostate cancer clinical trials: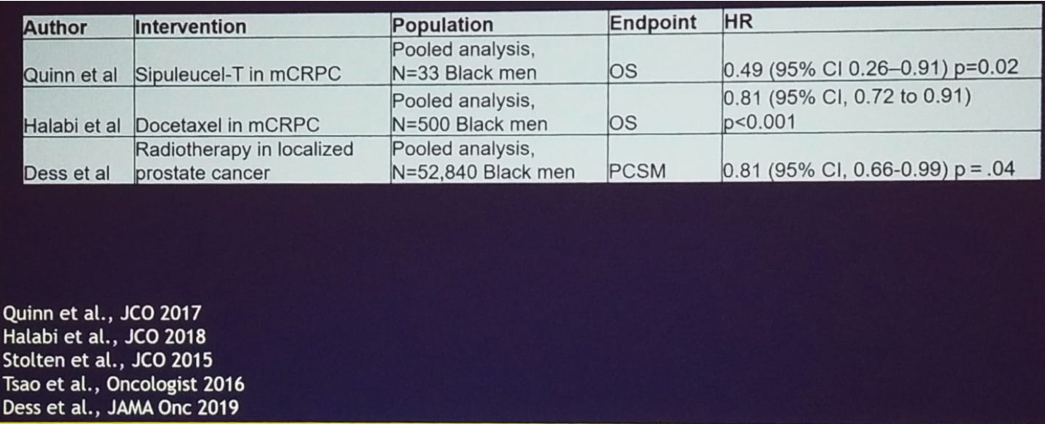
Presented by: Hala Borno, MD, BS, Hala Borno, MD Medical Oncologist and Assistant Professor of Medicine, University of California San Francisco, San Francisco, CA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2019 ASCO Annual Meeting #ASCO19, May 31- June 4, 2019, Chicago, IL USA
References:
- Spratt D. et al. JAMA ONC 2016
- Pritchard CC et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N Engl J Med 2016; 375:443-453.
- Galgano et al. Patient Demographics and Refeerral Patterns for [F-18]Fluciclovine-PET Imaging at a Tertiary Academic Medical Center. J Am Coll Radiol. 2019 Mar;16(3):315-320.
- Spratt et al. Disparities in castration-resistant prostate cancer trials. JCO 2015 Apr 1;33(10):1101-3.
- Balakrishnan et al. J. UROL 2019.
- Butler et al. Active Surveillance for Low-Risk Prostate Cancer for Black Patients. N Engl Med 2019; 380:2070-2072.


