In this prospective and randomized Phase II study, Enrique Grande, MD, and co-authors tested the hypothesis that a tumor inflammation score (TIS)1 could predict which patients with MIBC responded better to neoadjuvant ICB. They randomized patients based on inclusion criteria shown below based on their tumor inflammation score (hot = scoring in top two-thirds of distribution, cold = lower third of score distribution). “Cold” tumors were treated with standard of care neoadjuvant chemotherapy, and “hot” tumors were randomized 1:1 to either standard of care chemotherapy or the combination of the anti-PD-L1 antibody durvalumab and the anti-CTLA4 antibody tremelimumab. A safety run-in phase with six patients was built into the immunotherapy intervention arm. The primary outcome was pathologic complete response rate (pCR), and secondary outcomes were disease-free survival, overall survival, and toxicity.
The cohort characteristics are shown below.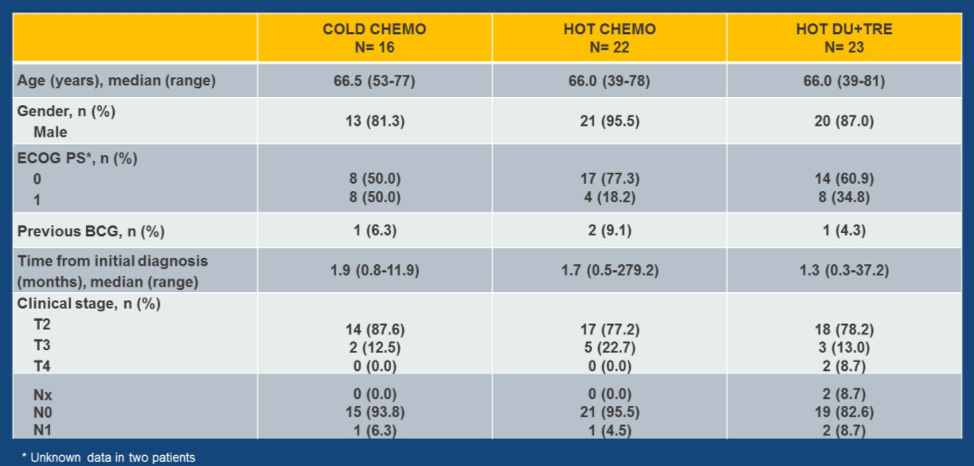
No unexpected toxicities were experienced in the chemotherapy arms. The most common toxicities in the immunotherapy arm were asthenia, diarrhea, and skin rash. In total, 21% of patients in the immunotherapy arm had Grade 3 or 4 toxicity of any type, whereas 47.4% of patients receiving chemotherapy experienced a Grade 3 or 4 treatment-related adverse event.
Of all patients in the chemotherapy arms, 50% in the “hot” tumor group and 41% in the “cold” tumor group completed all planned cycles of neoadjuvant therapy, whereas 78.3% of patients in the immunotherapy arm completed all planned cycles of therapy. Approximately 90% of patients in all three arms underwent cystectomy.
The response rates are shown below.
pCR rate did not differ by PD-L1 expression in the overall cohort, but rates did differ by PD-L1 expression in the “hot” tumors treated with immunotherapy as well as the “cold” tumors treated with chemotherapy.
PD-L1 expression was higher in “hot” tumors as classified by the TIS, and “hot” tumors with higher PD-L1 expression by combined immune score had higher rates of pCR.
Finally, pCR rates were found at all levels of TIS score.

In this Phase II study, the pCR rate in tumors selected by TIS score and treated with combined ICB was 34.8%. There was no clear advantage to selected tumors for therapy based on TIS score.
Presented by: Enrique Grande, MD, Head of Medical Oncology Service, MD Anderson Cancer Center Madrid, Madrid, Spain
Written by: Alok Tewari, MD, Ph.D., Medical Oncology Fellow at the Dana-Farber Cancer Institute, Boston, Massachusetts, at the 2020 American Society of Clinical Oncology Virtual Annual Meeting (#ASCO20), May 29th-May 31st, 2020
Reference:- Ayers, Mark, Jared Lunceford, Michael Nebozhyn, Erin Murphy, Andrey Loboda, David R. Kaufman, Andrew Albright et al. "IFN-γ–related mRNA profile predicts clinical response to PD-1 blockade." The Journal of clinical investigation 127, no. 8 (2017): 2930-2940.


