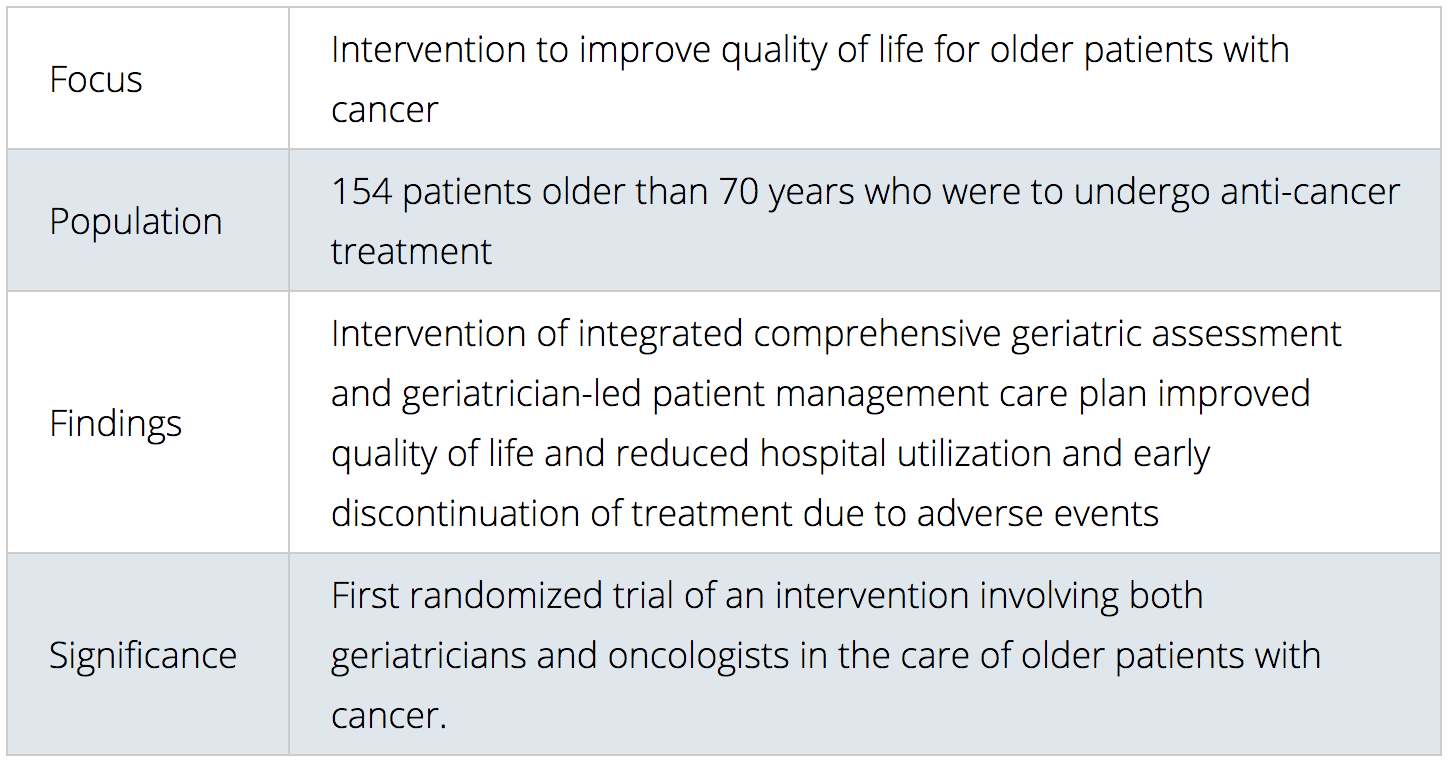
San Francisco, California (UroToday.com) — Older people with cancer set to receive anti-cancer therapy had significant improvements in quality of life when comprehensive geriatric assessment and geriatrician-led management was integrated into their care plan. The prospective, randomized, open-label INTEGERATE trial, according to the study authors, is the first randomized clinical trial in geriatric oncology to show that an integrated approach involving geriatricians and oncologists working in partnership helped improve quality of life, and reduced hospital admissions and early discontinuation of treatment due to adverse events.
Study at a Glance:
The findings will be featured in the virtual scientific program of the 2020 American Society of Clinical Oncology (ASCO) Annual Meeting.
Key Findings: Comprehensive geriatric assessment is a detailed systematic evaluation of an older person that identifies medical, psychosocial, and functional limitations. Currently, a person with cancer is typically referred to a geriatrician only in the later stages of their illness when they experience significant problems with completing everyday tasks. However, an integrated approach involving comprehensive geriatric assessment and early geriatrician involvement (also known as “integrated oncogeriatric care”) can help create a coordinated plan to optimize the older person with cancer.
“The comprehensive geriatric assessment is a powerful tool because it helps optimize care for older cancer patients,” said lead author Wee-Kheng Soo, MBBS, FRACP, who is a geriatrician and medical oncologist at Eastern Health in Melbourne, Australia.
The intervention resulted in improvement in more objective measures as well, including unplanned hospital admissions, and reduced early treatment discontinuation due to adverse events.
About the Study: The trial involved 154 patients with cancer older than 70 years who were going to receive chemotherapy, targeted therapy, or immunotherapy treatment. Patients were randomized to receive integrated oncogeriatric care or usual care.
The study’s primary outcome, quality of life, was measured using a validated assessment tool called the Elderly Functional Index (ELFI) score. Quality of life was also assessed using the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life of Questionnaire.
Patients in the intervention group reported significantly better ELFI scores at 12, 18, and 24 weeks of follow up, compared with the group receiving usual care. The greatest difference was seen at week 18 (estimated marginal mean ELFI score 72.0 in the intervention group vs. 58.7 in the group receiving usual care). In addition, the intervention group saw significant improvements in other quality of life measures, including functioning, mobility, burden of illness, and future worries.
Hospital utilization was reduced: there were 1.3 fewer visits to the emergency department per person per year (39% lower than the usual care group), and by 1.2 fewer unplanned hospital admissions per person per year (43% lower). The number of overnight stays also decreased by 7 days per person per year (24% lower). The proportion of patients discontinuing treatment early due to adverse events was lower than the group receiving usual care (32.9% vs. 53.2%). This decline appears to be driven by reduced treatment-related toxicity.
Next Steps: The researchers plan to implement an oncogeriatric model of care in a large, multi-center implementation study comparing different care models in geriatric oncology (e.g. geriatrician-led, nurse-led, oncologist-led) and different cancer settings (e.g. surgical oncology, radiation oncology, inpatient).
Source: ASCO. “Integrating Geriatric Assessment and Management Into Cancer Care Improves Quality of Life, Reduces Hospital Admissions for Older Patients,” May 8, 2020.
Related Content:
View all ASCO 2020 Virtual Scientific Program Coverage


