To further characterize the molecular associations with germline BRCA2, Dr. Lozano and colleagues conducted a multicenter, matched case-control study where gBRCA2 patients were matched 1:2 with non-carriers. BRCA1 germline mutation carriers were included as an exploratory cohort. The goal of this study was to confirm the independent prognostic value of gBRCA2 on prostate-cancer specific mortality, and secondarily, to examine molecular associations between gBRCA2 and copy number as assessed by FISH for BRCA2, RB1, MYC, PTEN, and TMPSS2-ERG fusion. The flowchart of the study is shown here.

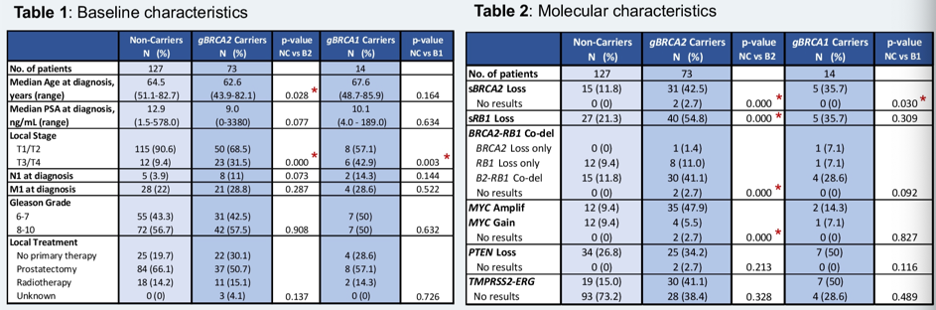
The clinical and molecular characteristics of patients in this study are shown below. Patients with prostate cancer and gBRCA2 were younger than other prostate cancer patients and tended to have T3/T4 disease at higher rates than other patients. gBRCA2 patients also had more copy number alteration, and higher frequency of BRCA2 loss, RB1 loss, and MYC amplification. BRCA1 germline mutated samples also had more copy number alterations, but not to a statistically significant degree compared to controls. gBRCA2 samples were also associated with BRCA2-RB1 genomic codeletion. These two genes are located near each other on chromosome 13q.
With regards to the impact of somatic and germline alterations on survival, gBRCA2 patients had lower prostate-cancer specific survival (PCSS) relative to BRCA1 germline mutation carrier or noncarriers (9.1 years versus 13.5 years versus 17.6 years, p = 0.004). gBRCA2 patients with BRCA2-RB1 somatic co-deletion had worse PCSS relative to gBRCA2 carriers. Similarly, gBRCA2 patients with MYC somatic amplification had lower PCSS relative to gBRCA2 carriers. Non-gBRCA2 patients with BRCA2-RB1 codeletion or MYC amplification also had a worse prognosis than non-gBRCA2 patients without these somatic changes.
In a multivariate model for PCSS including genomic status, age, PSA, Gleason score, nodal involvement, tumor stage, and de novo metastatic status, gBRCA2 status was an independent risk factor for PCSS. MYC amplification and BRCA2-RB1 deletion were also independent prognostic factors.

In summary, this study confirmed that germline mutation in BRCA2 is an independent prognostic factor for lower prostate cancer-specific mortality and is associated with more somatic aberrations including MYC amplification and BRCA2-RB1 deletion.
Presented by: Rebeca Lozano, MD, Clinical Research Fellow at the Prostate Cancer Clinical Research Unit of the Spanish National Cancer Research Centre (CNIO), Madrid, Spain
Related Content:
Warch: Influence of BRCA-2 Mutations on the Natural History and Response to Therapy in Prostate Cancer- Elena Castro


