Magnetic resonance imaging (MRI) has been gaining an increasingly large role in the management of patients with early-stage prostate cancer including diagnosis in patients with abnormal PSA levels, monitoring of patients on active surveillance, and staging before definitive interventions. MRI-based prostate cancer risk assessment has been shown to better distinguish between clinically significant and insignificant tumors than PSA testing alone or from nomograms.
The role of prostate MRI for screening, in an unselected population, is relatively untested. A small, single-center study from Toronto, Ontario, Canada piloted this approach among 47 men and compared the performance of MRI to that of PSA1. MRI outperformed PSA as a screening test in this small analysis.
In a Poster discussion session at the 2020 American Society of Clinical Oncology Virtual Annual Meeting, Dr. Eldred-Evans and colleagues presented the results of the IP1-PROSTAGRAM study which evaluates the performance of a 15-minute non-contrast MRI for prostate cancer screening in comparison to PSA.
In a prospective, population-based, screen-positive paired-cohort study, the authors recruited men aged 50-69 years in the UK for prostate cancer screening through seven primary care practices or community-based recruitment. All participants underwent a PSA and MRI scan (T2-weighted and diffusion). MRI was scored using PIRADS version 2.0 without knowledge of PSA.
Patients with a PIRADS score 3-5 or 4-5 were considered “screen-positive” as this definition was compared against the performance of PSA with a “screen-positive” PSA defined as ≥3ng/ml. Where men were identified as “screen-positive” by either MRI or PSA results, patients underwent a systematic 12-core biopsy was performed with MRI-ultrasound image-fusion targeted biopsy to MRI suspicious areas, as appropriate.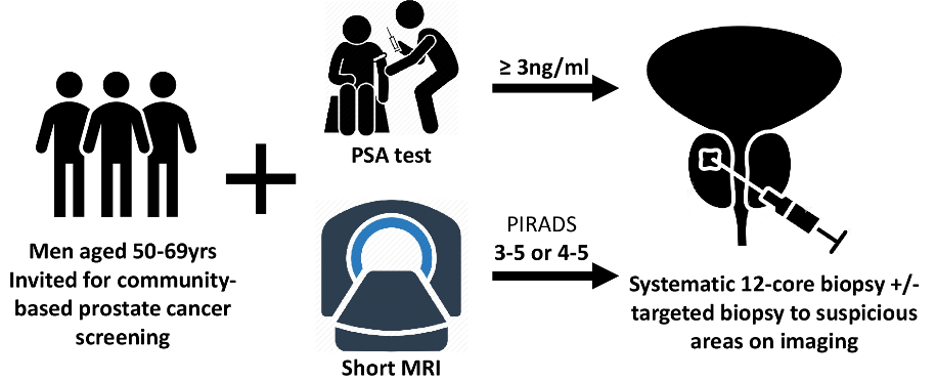
The authors defined clinically-significant cancer as any Gleason score ≥3+4. The primary outcome was the proportion of screen-positive MRI at different scores thresholds (3-5 vs 4-5). Key secondary outcomes were the number of clinically-significant and insignificant cancers detected.
The authors invited 2034 men to participate of whom 408 consented and 406 were screened by both PSA and MRI between 10 Oct 2018 and 15 May 2019.
MRI using a “screen-positive” definition of 3-5 was associated with a higher rate of abnormality detection (17.7%, 95% confidence interval 14.3 to 21.8%) compared to a PSA threshold of 3ng/mL (9.9%, 95% confidence interval 7.3 to 13.2%; p<0.001), suggestive of higher sensitivity. When a “screen-positive” definition of 4-5 was used, results were comparable between MRI (10.6%, 95% confidence interval 7.9 to 14.0%) and PSA (9.9%, 95% confidence interval 7.3 to 13.2%; p=0.71).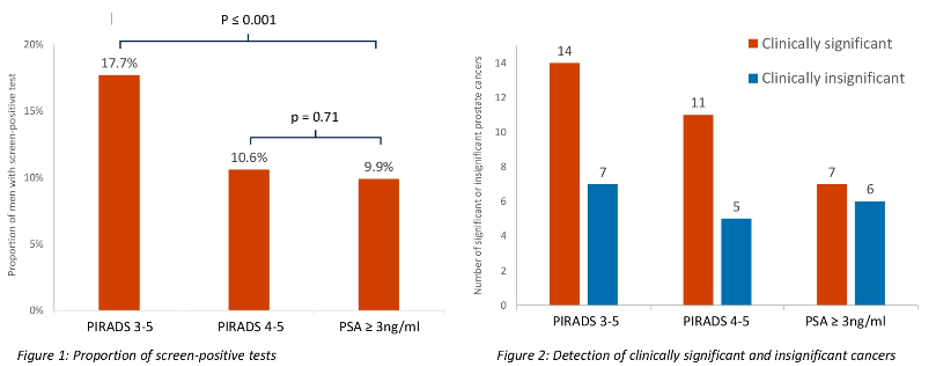
Clinically significant prostate cancer was detected in 14 patients with MRI score 3-5, 11 of those with an MRI score 4-5, and 7 of those with abnormal PSA. In contrast, clinically insignificant cancers were detected in 7 patients with MRI score 3-5, 5 of those with an MRI score 4-5, and 6 of those with abnormal PSA.
The authors concluded that the use of MRI with a “screen-positive” definition of PIRADS 4-5, when compared to PSA based screening using a threshold of 3ng/mL, was associated with increased rates of diagnosis of clinically significant prostate cancer without increasing diagnosis of clinically insignificant disease.
Presented by: David Eldred-Evans, MBBS, Imperial Research Fellow, Department of Surgery & Cancer, Imperial College of London
Co-Authors: Paula Burak, Martin John Connor, Emily Day, Martin Evans, Francesca Fiorentino, Martin Gammon, Feargus Hosking-Jervis, Natalia Klimowska- Nassar, William McGuire, Anwar R Padhani, Derek Price, Toby Prevost, Heminder Sokhi, Henry Tam, Mathias Winkler, Hashim Uddin Ahmed
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter at the 2020 American Society of Clinical Oncology Virtual Annual Meeting (#ASCO20), May 29th-May 31st, 2020
References:


