(UroToday.com) As part of the American Society of Clinical Oncology (ASCO) 2021 Annual Meeting, a session entitled “Breaking Barriers: Ensuring Equity in Cancer Diagnosis, Treatment, and Trial Enrollment for Patients with Kidney and Bladder Cancers”, Dr. Hoffman-Censits presented on bladder cancer in women.
Dr. Hoffman-Censits began by emphasizing that bladder cancer is more common in men than in women: it is the 4th most commonly diagnosed cancer in men and the 8th leading cause of cancer-related death. In contrast, in women, are much less likely to be diagnosed with bladder cancer. However, among those who are diagnosed with bladder cancer, mortality rates are higher for women than men. This is a finding that she emphasized is unique among solid tumors.
She then highlighted a number of factors underpinning these sex-based disparities in bladder cancer including the management of presentations with hematuria symptoms; the completeness of evaluation; the stage at presentation; the age at presentation; the provision of and response to therapy; and underlying tumor biology.
While the most common presenting symptom of bladder cancer for both men and women is either microscopic hematuria or gross hematuria, the work up is not equal for men and women: the median time from presentation to cystoscopic evaluation is nearly two weeks longer for women (72.2 days compared with 58.9 days). Along the way, women are more likely to undergo more urine cultures, be prescribed more courses of antibiotics, and be referred to non-urologist specialties.
In terms of evaluation quality, consistently, complete evaluation (including urologic consultation, endoscopic evaluation, and imaging) is quite poor. However, women and particularly Black women were less likely to undergo complete evaluation than men.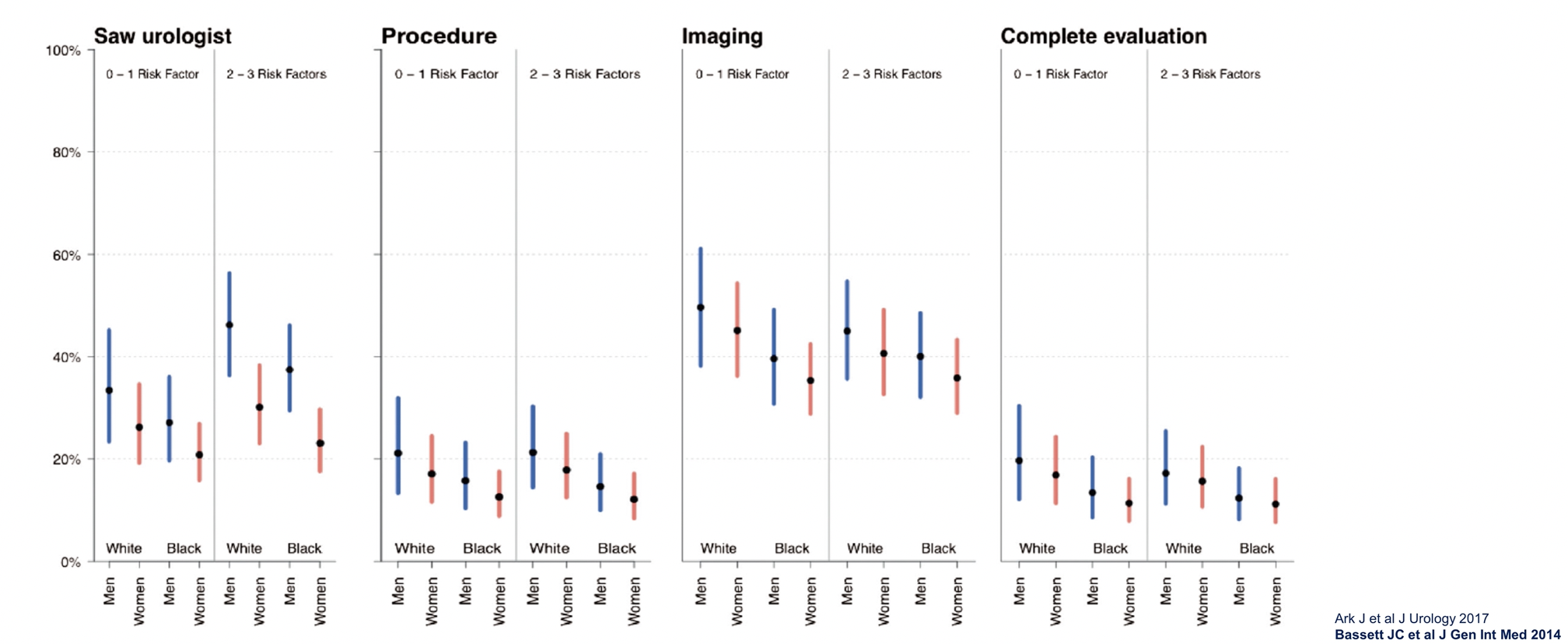
Incomplete evaluation has important consequences – it may lead to stage inaccuracy which in turn affects outcomes. Prior work from Dr. Chamie has shown that five-year mortality is increased for patients with bladder cancer who do not have muscle appropriately sampled in the specimen. This effect is even larger among patients with high-grade disease. Further, in this analysis, the authors found that patients with substandard staging were more likely to be women and women of color.
While the underlying cause is not entirely clear (and may result from diagnosis delay, inadequate staging, or tumor biology), women consistently present with bladder cancer at more advanced stages than men, with higher proportions of muscle-invasive and metastatic disease. These disparities are even more profound among Black women.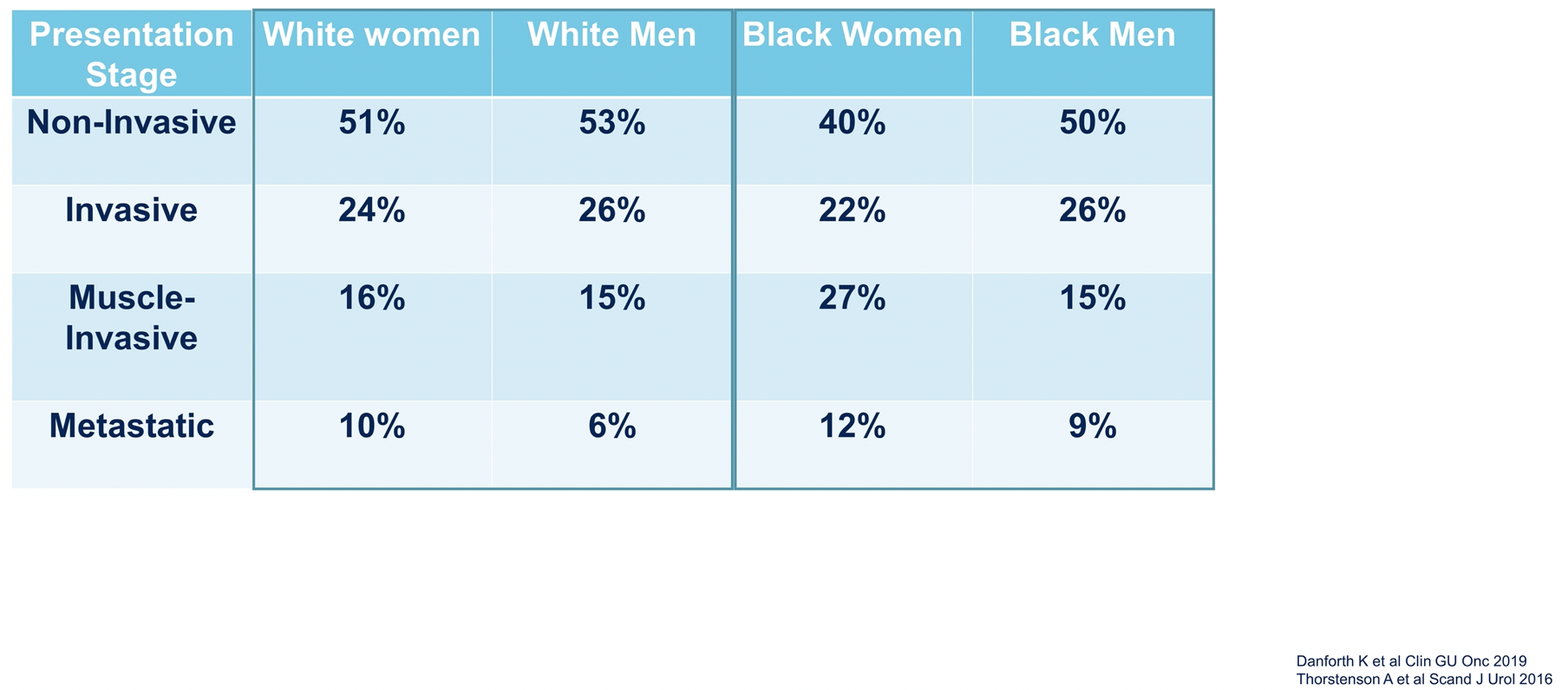
Further, women are also older at the time of bladder cancer diagnosis. This may affect clinical decision-making and the provision of curative intent therapy. However, among women who receive chemotherapy, there is no difference in overall survival for women and men receiving chemotherapy for bladder cancer based on pooled data from a number of clinical trials.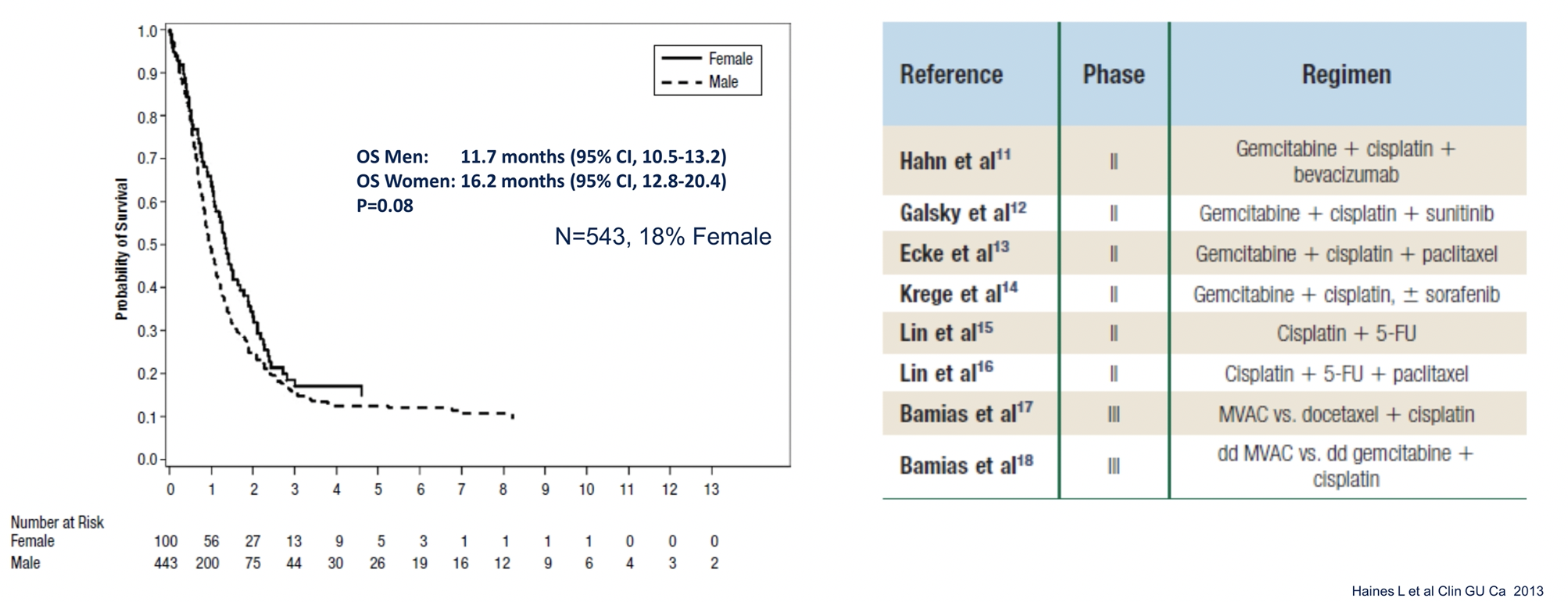
However, outside the context of clinical trials, women are less likely to receive chemotherapy for metastatic urothelial carcinoma based on an analysis of nearly 24,000 patients identified in the National Cancer Database: 45% of women and 52% of men received systemic chemotherapy (relative risk 0.86, 95% CI 0.83-0.88). Even adjusting for age, year of diagnosis, race, insurance status, distance to and location of treatment facility, income, education, facility type, comorbidity, histology, cystectomy, and clinical T and N stage, the effect persisted (RR 0.91, 95% CI 0.88-0.94). Perhaps not surprisingly, women had lower median overall survival (8.0 months, 95% CI 7.7-8.3 months) than men (9.8 months, 95% CI 9.5-10.0 months) (p<0.001).
However, in response to neoadjuvant chemotherapy, women and men had similar pathologic complete response and downstaging. However, women were less likely to have tumors with DNA damage repair gene mutations than men (28% vs 45%, p<0.001). In this retrospective study of patients who received neoadjuvant therapy, there was no difference in overall or cancer specific mortality.
Among a number of cohorts of patients on clinical trials of atezolizumab in advanced bladder cancer, Dr. Hoffman-Censits highlighted that men may have higher objective response rates in all trials, except for the first line, though none of these reach significance.
She emphasized that an understanding of sex-based differences in tumor biology remains a fertile area for ongoing research as this is poorly understood. Basal and luminal subtypes of bladder cancer have been appreciated in recent years and it is understood that this division has important prognostic importance. Women with bladder cancer tend to have tumors fitting within the basal/squamous subtype which may have important implications for sensitivity to systemic therapy.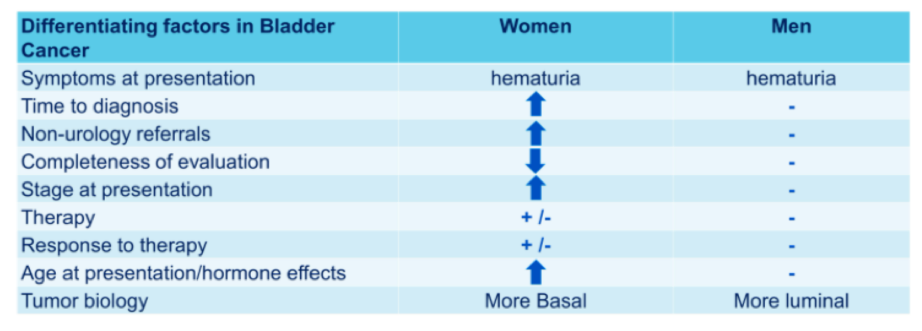
She concluded that, in summary, men and women present with similar symptoms though, from that time forward, women often experience delays in therapy and less provision of curative care though responses to treatment are likely similar emphasizing the value of providing appropriate care to women with bladder cancer.
Presented by: Jean H. Hoffman-Censits, MD, Co-leader, Women’s Bladder Cancer Program, Greenberg Bladder Cancer Institute, Assistant Professor of Oncology, Johns Hopkins Medicine
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Contact: @WallisCJD on Twitter at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


