Dr. Singer notes that many patients present with advanced disease at the time of diagnosis, with established roles for cytoreductive surgery among patients with ovarian, colorectal, and breast cancer. However, there are often conflicting outcomes seen in prospective trials and observational studies. In a previously published systematic review, Bhindi et al.1 assessed whether cytoreductive nephrectomy versus no cytoreductive nephrectomy was associated with improved overall survival (OS) in patients with mRCC treated in the targeted therapy era and beyond. They found that cytoreductive nephrectomy was associated with improved OS among patients with mRCC in 10 nonrandomized studies, while one randomized trial (CARMENA2) found that OS with sunitinib alone was non-inferior to that with cytoreductive nephrectomy followed by sunitinib. Notably, 12.9-30.4% of patients did not receive systemic therapy after cytoreductive nephrectomy. Good performance status and good/intermediate IMDC/MSKCC risk classification were most consistently predictive of OS benefit with cytoreductive nephrectomy. In a randomized trial investigating the sequence of cytoreductive nephrectomy and systemic therapy (SURTIME3), an OS trend was observed with cytoreductive nephrectomy after a period of systemic therapy in patients without progression compared with upfront cytoreductive nephrectomy.
To assess the impact of cytoreductive nephrectomy in the immunotherapy era, Singla et al.4 used the NCDB to evaluate survival outcomes, timing, and safety of combining cytoreductive nephrectomy with modern immunotherapy for mRCC. Among 391 patients, 221 (56.5%) received cytoreductive nephrectomy + immunotherapy and 170 (43.5%) received immunotherapy only. Over a median follow-up of 14.7 months, patients who underwent cytoreductive nephrectomy + immunotherapy had superior OS (median NR vs. 11.6 months; hazard ratio 0.23, p < 0.001):

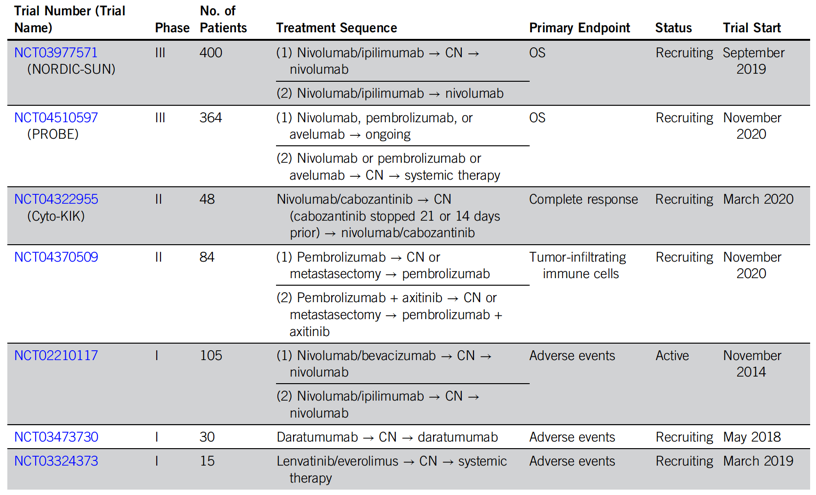
Dr. Singer notes that there are several ongoing clinical trials investigating cytoreductive nephrectomy or metastasectomy with systemic therapy,5 as highlighted in the following table:
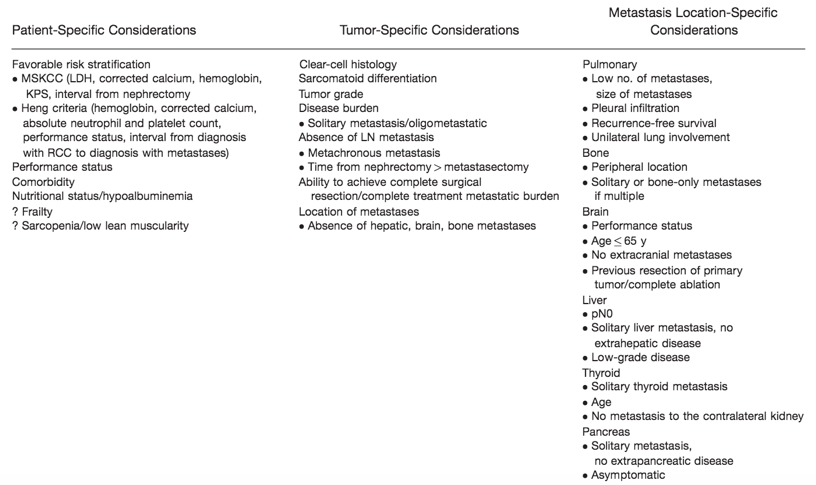
Metastasectomy includes the surgical resection of metastatic disease, which can be high risk/high reward and must include careful tumor staging and patient selection. As highlighted in a review by Psutka and Master,6 there are several prognostic factors that may be taken into consideration when selecting and counseling patients regarding definitive treatment of renal cell carcinoma metastases:
A study from the Canadian Kidney Cancer information system database assessed the impact of complete metastasectomy in mRCC patients using real-world pan-Canadian data.7 There were 229 patients that underwent complete metastasectomy who were matched with 803 patients not treated with metastasectomy. After 12 months, the proportion of patients that were still alive was 96.0% and 89.8% in the complete metastasectomy and its matched group, respectively, with a 5-year OS rate of 63.2% for those undergoing metastasectomy and 51.4% for controls:
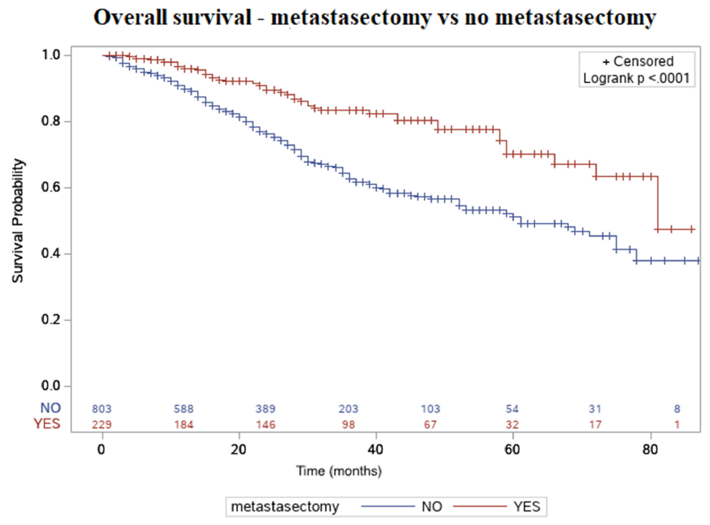
Furthermore, patients older than 65 years of age (HR 2.47, 95% CI 1.64-3.73) and patients with brain metastases (HR 6.90, 95% CI 1.23-38.2) had an increased risk of mortality in this cohort.
To assess the impact of metastasectomy in RCC in the postcytokine therapy era, Ishihara et al.8 utilized institutional data from several Japanese centers. Among 314 patients over a median follow-up of 25.3 months, 98 patients (31.2%) underwent at least one metastasectomy. Patients undergoing complete metastasectomy (n = 45, 14.3%) had a significantly longer OS (median not reached) compared to those undergoing an incomplete metastasectomy (n = 53, 16.9%) (median 81.5 months, p = 0.0042) and those not undergoing metastasectomy (median 28.1 months, p < 0.0001):
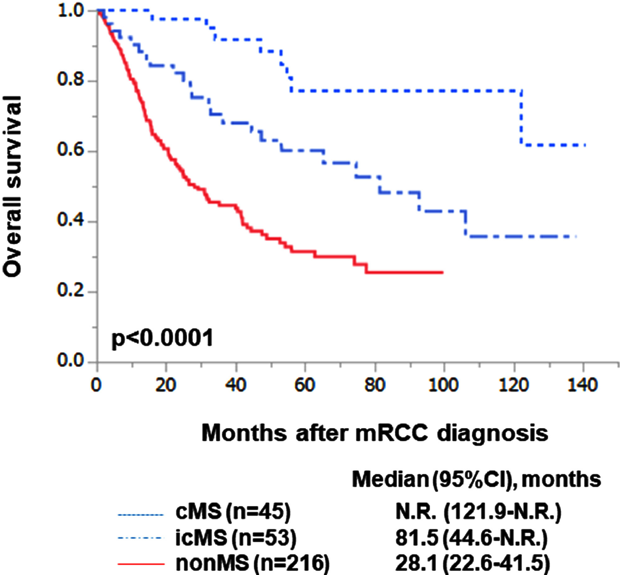
Additionally, OS was comparable throughout the eras of systemic therapy (early molecular-targeted therapy, late molecular-targeted therapy, and immune checkpoint inhibitor eras) in the metastasectomy group (median: 121.9 months vs not reached, p = 0.948).
Recently, stereotactic ablative radiation therapy has been assessed in order to defer systemic therapy for patients with oligometastatic RCC. Using data from the UT Southwestern Kidney Cancer database, Zhang et al.9 evaluated the potential of stereotactic ablative radiation therapy for longitudinal control in 47 patients with persistently oligometastatic RCC. Among these patients, stereotactic ablative radiation therapy was used to treat 88 metastases, with a local control rate of 91.5% at 2 years and no reported grade ≥3 toxicity. Over a median follow-up of 30 months (IQR, 13.7-40.9), median freedom from systemic therapy from first stereotactic ablative radiation therapy was 15.2 months (95% CI 8.8-40.1). Improved freedom from systemic therapy was observed in patients with metachronous disease (HR 2.67, p = 0.02), solitary metastasis (HR 2.26, p = 0.05), and non-bone metastasis (HR 2.21, p = 0.04). Additionally, 1-year and 2-year OS after stereotactic ablative radiation therapy were 93.1% (95% CI, 80.1-97.7) and 84.8% (95% CI, 69.1-92.9), respectively.
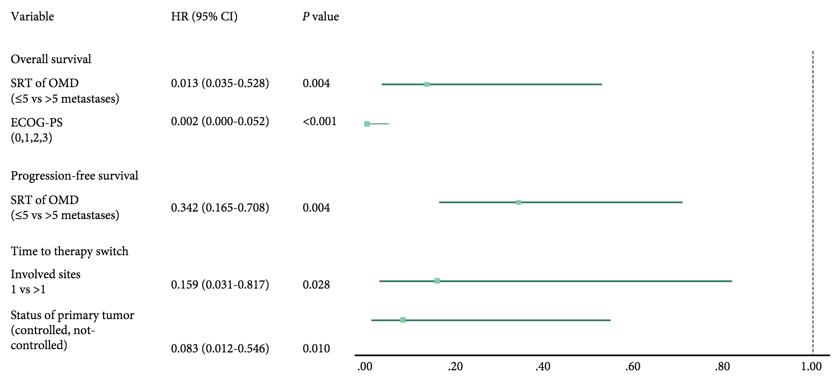
To evaluate the safety and efficacy of stereotactic radiotherapy in patients with mRCC concurrently receiving targeted therapy or immunotherapy, Kroeze et al.10 used an international multicenter registry to identify 53 patients who underwent 128 sessions of stereotactic radiotherapy. Immune checkpoint inhibitors and targeted therapy were received by 32% and 68% of patients, respectively. The OS, local control, and PFS rates at 1 year were 71%, 75%, and 25%, respectively. Furthermore, the median OS and PFS were not significantly different among patients receiving targeted therapy vs those receiving immune checkpoint inhibitors (p = 0.329). After 1 year, 62% of patients remained on the same systemic therapy as at the time of stereotactic radiotherapy. Oligometastatic disease was an independent prognostic factor for OS and PFS in multivariate analysis:
Dr. Singer concluded his presentation by highlighting that optimal patient selection for treatment is key, including taking into consideration performance status, burden of disease (inside/outside the kidney; number of sites), the sites of disease (brain/bone), and the timing of systemic therapy/type (monotherapy versus combination therapy).
Presented by: Eric A. Singer, MD, FASCO, FACS, MA, MS | Section of Urologic Oncology, Rutgers Cancer Institute of New Jersey and Rutgers Robert Wood Johnson Medical School
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021
References:
- Bhindi B, Abel EJ, Albiges L, et al. Systematic review of the role of cytoreductive nephrectomy in the targeted therapy era and beyond: An Individualized Approach to Metastatic renal cell carcinoma. Eur Urol 2019 Jan;75(1):111-128.
- Mejean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal cell carcinoma. N Engl J Med 2018 Aug 2;379(5):417-427.
- Bex A, Mulders P, Jewett M, et al. Comparison of immediate vs deferred cytoreductive nephrectomy in patients with synchronous metastatic renal cell carcinoma receiving sunitinib: The SURTIME Randomized Clinical Trial. JAMA Oncol 2019 Feb 1;5(2):164-170.
- Singla N, Hutchinson RC, Ghandour RA, et al. Improved survival after cytoreductive nephrectomy for metastatic renal cell carcinoma in the contemporary immunotherapy era: An analysis of the National Cancer Database. Urol Oncol. 2020 Jun;38(6):604.e9-604.e17.
- Schmidt AL, Tabakin AL, Singer EA, et al. Next Steps: Sequencing therapies in metastatic kidney cancer in the contemporary era. Am Soc Clin Oncol Educ Book. 2021 Mar;41:1-11.
- Psutka SP, Master VA. Role of Metastasis-Directed Treatment in Kidney Cancer. Cancer. 2018 Sep 15;124(18):3641-3655.
- Dragomir A, Nazha S, Wood LA, et al. Outcomes of complete metastasectomy in metastatic renal cell carcinoma patients: The Canadian Kidney Cancer information system experience. Urol Oncol. 2020 Oct;38(10):799.e1-799.e10.
- Ishihara H, Takagi T, Kondo T, et al. Prognostic impact of metastasectomy in renal cell carcinoma in the postcytokine therapy era. Urol Oncol. 2021 Jan;39(1):77.e17-77.e25.
- Zhang Y, Schoenhals J, Christie A, et al. Stereotactic Ablative Radiation Therapy (SAbR) Used to Defer Systemic Therapy in Oligometastatic Renal Cell Cancer. Int J Radiat Oncol Biol Phys. 2019 Oct 1;105(2):367-375.
- Kroeze SGC, Fritz C, Schaule J, et al. Stereotactic radiotherapy combined with immunotherapy or targeted therapy for metastatic renal cell carcinoma. BJU Int. 2020 Oct 28 [Epub ahead of print].


