Dr. Robert Given has posed the question on this case of whether one can extrapolate the data supporting radiotherapy to the primary prostate tumor in low volume metastatic disease (by CHAARTED criteria) to advocate for prostatectomy in this context. He cited retrospective data of less than 100 men who underwent prostatectomy in the context of M1b disease as well as androgen deprivation therapy, and at three-year follow-up, the cancer-specific survival was 92%. Dr. Given noted that there was a significant rate of urinary side effects in these patients (> 20% of patients using 2 pads or more per day), and this data was not randomized prospective data, and ultimately concluded that the data is not clear yet on the utility of prostatectomy in this setting. More commonly in the U.S., since PSMA-PET scan prior to definitive management is not common now, a patient is diagnosed with metastatic disease by conventional imaging. In that context, especially outside the context of a clinical trial, Dr. Given does not typically advocate for prostatectomy. One caveat to that statement might be a patient with significantly lower urinary tract symptoms (LUTS) from whom radiotherapy would be very detrimental to urinary symptoms whereas surgery would relieve the cause of the LUTS.
Case 2: 66M who underwent robotic prostatectomy and standard pelvic lymph node dissection for pT2cN0M0 Gleason 4 + 4 adenocarcinoma. Post-op PSA was detectable at 0.04 and rose to 1.0 over the next year. CT and bone scan were negative, but a sodium fluoride PET scan showed a bony metastatic lesion to the 9th right rib. The patient was treated with 3000 cGy to the rib with a short course of androgen deprivation therapy. After two years of undetectable PSA, the patient’s PSA rose to 1.6 ng/mL. A fluciclovine PET/CT was obtained, which showed a left pelvic nodal area of avidity.
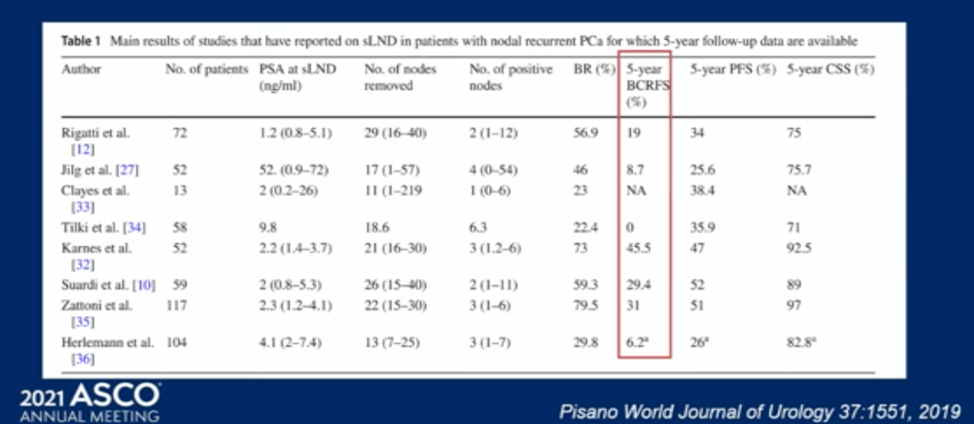
Dr. Given discussed whether salvage lymphadenectomy for pelvic nodal recurrence might be feasible in this case. This is an approach supported only by several retrospective series. There are many open questions for such an approach including how extensive the lymph node dissection should be, and which patients are optimal candidates for such an approach. This surgery can be done as an open, laparoscopic, or robotic surgery with tolerable rates of complications generally consisting of ileus, deep vein thrombosis, or lymphocele formation. The Clavien grade 3 complication rates for salvage lymph node dissection in the literature ranges from 0-27%. The available evidence suggests that patients are likely to at least have a PSA response from salvage lymphadenectomy and the rates of biochemical relapse-free survival range in the literature from 0-45% at five years. Patients with PSA less than 4 and no evidence of retroperitoneal disease seem to have higher rates of recurrence-free survival. Prospective studies are needed to further clarify the role of salvage lymphadenectomy in oligometastatic lymph node disease.
Case 3: 66M with cT2cN1M0 Gleason 5+4 in 12/12 biopsy cores, PSA 14 ng/mL who was initially treated with radiotherapy and long-term ADT. For two years after initial therapy, his PSA remained in the 0.7-1.3 ng/mL range, but then rose to 5.4 ng/mL despite testosterone level less than 20. Imaging showed new bulky > 2.5 cm left-sided para-aortic and RP nodes.
Dr. Given noted that there is ongoing research as to whether surgical salvage may be an option for cases like this.
Presented by: Robert Given, MD, FACS, community urologist in Virginia Beach, VA
Written by: Alok Tewari, MD, PhD, Medical Oncologist at the Dana-Farber Cancer Institute, at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


