This study included molecular profiling analysis of 1,375 cases of metastatic prostate cancer. Tumors were analyzed using next-generation sequencing, whole transcriptome sequencing, and immunohistochemistry (Caris Life Sciences, Phoenix, AZ). dMMR/MSI-H status was determined by immunohistochemistry, next-generation sequencing, and fragment analysis, and tumor mutational burden was calculated based on somatic nonsynonymous missense mutations. Differential gene expression analysis was performed of HR-associated transcripts such as ATR, PARP1-3, RAD50, RAD51A/B/C/D, and RAD54. Significance was determined using the chi-square test and the Benjamini-Hochberg method.
Fifty-nine (4.2%) cases harbored pathogenic ATM mutations, and 84 (6.2%) harbored BRCA2 mutations. There were 1,018 tumors (74%) deemed homologous recombination proficient (HRP) and 155 tumors (11.3%) were HR Deficient (HRD); harboring one or more mutations in HR-related genes excluding ATM and BRCA2. The mutation rate of TP53 was significantly lower in ATM mutant prostate cancer (12.0%) compared to BRCA2 mutant prostate cancer (35%), HRD (35%), and HRP (46.6%) tumors:
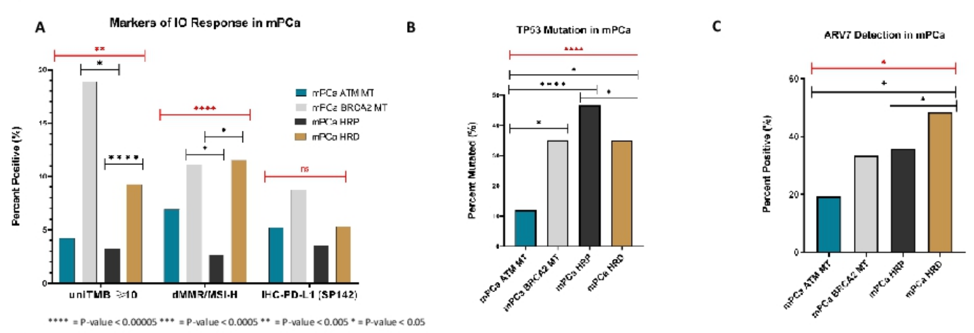
ATM mutant prostate cancer showed higher rates of SMAD2 (3.7%/1%) and FLCN (5.2%/0.3%) alterations compared to HRP cases. PARP1 and RAD51D gene expression was reduced in ATM mutant prostate cancer compared to HRP (p < 0.05) and BRCA2 mutant prostate cancer (p < 0.05) tumors, respectively. No differences in gene expression levels were detected for ATR, PARP2, PARP3, RAD50, and RAD54. Chromosomal segments demonstrating differential copy number alteration in ATM mutant prostate cancer versus HRP, HRD, or BRCA2 mutant prostate cancer included FGF19, FGF4, PTPN11, ALDH2, DAXX, BCL7A, CCND1, BMPR1A, and MEF2B (Q-value < 0.05 determined by chi-square). The most common copy number alteration in ATM mutant prostate cancer was CCND1, present in approximately 13% (7/55) of cases. Compared to BRCA2 mutant prostate cancer and HRD cases, ATM mutant prostate cancer cases are less likely to display markers of immunotherapy response such as dMMR/MSI-H or TMB ≥10 mutations/MB.
Dr. Ryan concluded his presentation with the following take-home messages:
- ATM mutant prostate cancer demonstrated several differences in co-occurring alterations compared to BRCA2 mutant prostate cancer, HRD and HRP metastatic prostate cancer
- ATM mutant prostate cancer tumors were less likely to harbor alterations in TP53 compared to BRCA2, HRD or HRP tumors
- Copy number alterations in ATM mutant prostate cancer occurred in 9 genes across distinct metastatic prostate cancer molecular subtypes and were enriched for those associated with the 11q13 amplicon harboring Cyclin D1
- The FGF and PTPN11 related pathways are potentially targetable pathways in ATM mutant prostate cancer and may merit further study
Future directions include multi-omic approaches to further characterize ATM and BRCA2 loss in prostate cancer, and novel therapeutic strategies that account for mechanistic differences between patients with ATM-mutated and other HRD mutations may improve outcomes in this population.
Presented by: Charles J. Ryan, MD, Division of Hematology, Oncology and Transplantation, Department of Medicine, University of Minnesota, Minneapolis, MN
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


