mCRPC patients (N = 137) with deleterious ATM or BRCA2 mutations who received taxanes, PARP inhibitors, or both (for >= 21 days) were identified from 9 US academic centers. Demographic, treatment, and survival data were collected. The primary outcome was time to PSA or clinical/radiologic progression (earlier of two), which was termed PFS. Kaplan-Meier analyses were performed for time-to-treatment-discontinuation, as well as overall survival (OS), from time of first taxane or PARP inhibitor therapy. Cox hazard ratio regression analyses were performed, adjusting for Gleason sum (≤7 versus 8-10). For OS, receipt of subsequent therapies following first taxane or PARP inhibitor was also included as a covariate.
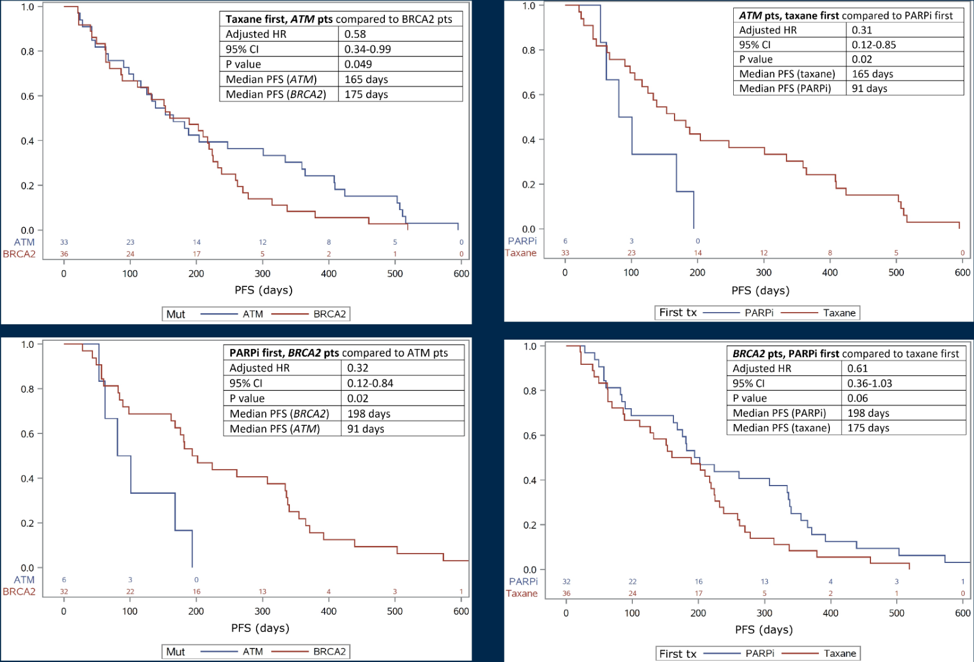
There were 50 ATM- and 87 BRCA2-mutated patients identified. Among the 50 ATM-mutated patients, 40 patients (80%) received taxane only or taxane prior to PARP inhibitor, while 10 patients (20%) received PARP inhibitors only or PARP inhibitors prior to taxane. ATM-mutated patients showed a trend towards longer time-to-treatment-discontinuation when taxane was given first versus PARP inhibitors given first (p = 0.08, adjusted HR for taxane treatment 0.50, 95% CI 0.24–1.08). Considering all patients who received taxane first, ATM-mutated patients had a longer time-to-treatment-discontinuation than BRCA2-mutated patients who received taxane first (p = 0.04, adjusted HR for ATM 0.61, 95% CI 0.37–0.99). Among ATM-mutated patients, OS was longer in those receiving taxane first (p = 0.06, adjusted HR for taxane treatment 0.33, 95% CI 0.10–1.05). Among BRCA2-mutated patients, 43/87 (49%) received taxane first and 44/87 (51%) received PARP inhibitors first. BRCA2-mutated patients had longer time-to-treatment-discontinuation when PARP inhibitor was given first vs taxane given first (p < 0.0001, adjusted HR for PARP inhibitor treatment 0.32, 95% CI 0.19–0.56). Considering all patients who received PARP inhibitor first, BRCA2-mutated patients also had longer time-to-treatment-discontinuation than ATM-mutated patients who received PARP inhibitor first (p = 0.0031, adjusted HR for BRCA2 0.29, 95% CI 0.12–0.66). There was no significant OS difference in BRCA2-mutated patients regarding which treatment was given first (p = 0.63, adjusted HR for PARP inhibitor treatment 1.18, 95% CI 0.59–2.35).
Dr. Su concluded this presentation with the following summary points:
- This data in ATM-and BRCA2-mutated mCRPC patients suggests a trend towards improved clinical outcomes when taxanes are used prior to PARP inhibitor in ATM-mutated patients, while the reverse sequence appears to be better for BRCA2-mutated patients
- Future directions include analysis of OS, development of more robust multivariable models, and analysis of other co-mutations present in identified patients
Presented by: Christopher T. Su, University of Michigan Rogel Cancer Center, Ann Arbor, MI
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


