(UroToday.com) There has been a proliferation in treatment options for patients with metastatic castration-resistant prostate cancer (mCRPC) in the last 10 years. While the most commonly utilized approaches in prostate cancer are cytotoxic chemotherapy or target the androgen-axis, recently, theranostic treatment with the PSMA-targeting radioligand therapy Lu-177 PSMA has demonstrated promising activity among pre-treated individuals with mCRPC. While there are many available treatment options, to date, we have been unable to widely operationalize rationale treatment selection in this disease space. In the Prostate, Testicular, Penile Poster session at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Dr. Stangl-Kremser and colleagues assessed the utility of PSMA protein expression in metastatic tumor tissues as a predictor of lesion-specific response to Lu-177 PSMA therapy in men with CRPC.
To do so, they examined 19 patients with metastases at multiple sites who underwent metastatic lesion biopsy, Ga-68 PSMA PET imaging, and treatment with three cycles of Lu-177 PSMA between 2015 and 2020. The authors semi-quantitatively assessed PSMA protein expression from the biopsy specimen using a monoclonal anti-PSMA antibody (EPITOMICS (USA), 1:50). The intensity and extent of the immunohistochemistry staining was assessed by experienced genitourinary pathologists to derive a histoscore (range 0-300). Ga-68 PSMA PET imaging was evaluated to the Positron Emission Tomography Response Criteria in Solid Tumors (PERCIST) criteria. Analytically, the authors considered the association between PSMA protein expression in biopsied metastatic tumor tissues and the lesion-specific response to Lu-177 PSMA therapy.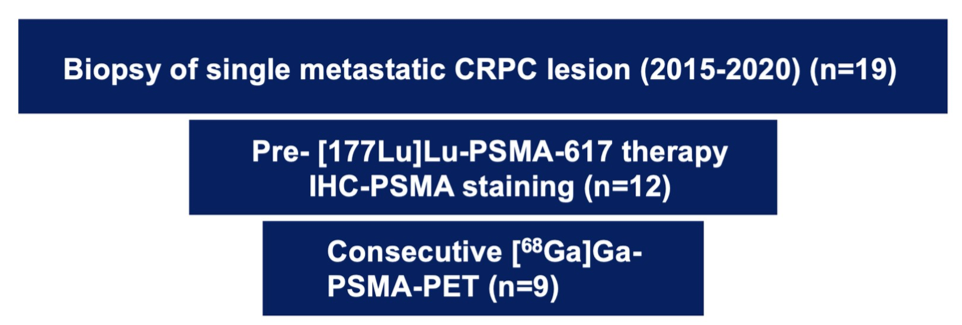
Among 19 patients initially considered, 12 patients had biopsy specimens available for staining. The median age of included patients was 67.4 years (IQR 64-72) and 92% had ECOG 0-1.The median SUVmax in the biopsied metastasis was 18.4 (IQR 11.1-29.5).
Among these 12 men, PSMA expression in the metastatic lesion on biopsy histology was correlated with enhancement (SUVmax) on Ga-68 PSMA PET imaging (rs = 0.63). Nine patients had repeat PSMA-PET/CT imaging after Lu-177 PSMA therapy, five of whom (55.6%) had a lesion-specific response at the site of biopsy.
In univariable analysis, PSMA expression on immunohistochemistry was not associated with lesion-specific response to Lu-177 PSMA (p = 0.8) or PSA decline (p=0.1). In the five men with a lesion-specific response, three (60%) experienced overall progression based on PERCIST though there was no association between lesion-specific response and overall progression (p = 0.64).
The authors conclude that histologic assessment of PSMA protein expression from a single metastatic site was associated with SUVmax on diagnostic PSMA-PET/CT but is not associated with site-specific Lu-177 PSMA response based on PERCIST.
Presented by: Judith Stangl-Kremser, MD, Department of Urology, University of Michigan
Written by: Christopher J.D. Wallis, MD, Ph.D., Urologic Oncology Fellow, Vanderbilt University Medical Center, Twitter: @WallisCJD at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting #ASCO21, June, 4-8, 2021


