
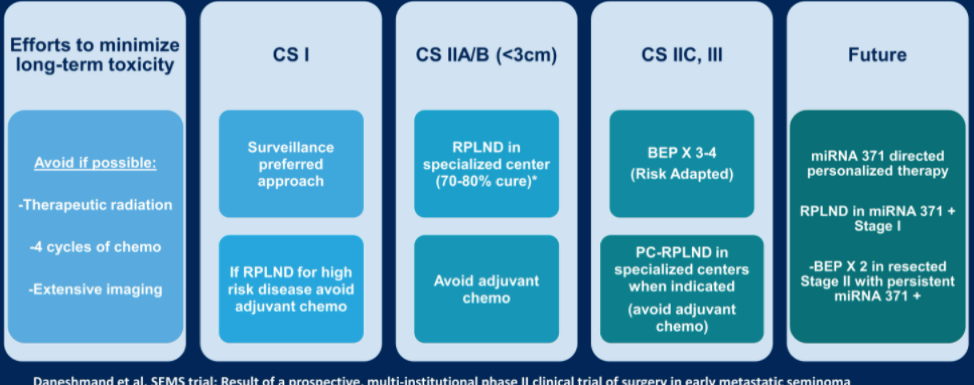
The first study used patients diagnosed with testicular cancer in Norway between 1980 and 2009. This cohort of 5,707 patients contained 665 survivors who had died from other causes. In total, the excess mortality in these patients over the general population was estimated at 23%, which was attributed to chemotherapy or radiotherapy treatment, but not surgery. The standardized mortality ratio in testicular cancer survivors increased with time, and the most common cause of death was related to secondary cancers. Importantly, patients who received cisplatin-based chemotherapy also had a higher risk of death due to suicide. Also of note, in this cohort, long-term cardiovascular mortality was not increased, and the risk of excess mortality from chemotherapy was highest in patients who received four or more cycles of therapy. Dr. Daneshmand concluded that his takeaway from this study is to avoid chemotherapy whenever possible. He offered the following general management scheme for reducing the risk of long-term toxicity, with emphasis on avoiding adjuvant chemo in clinical stage 1. He noted that the microRNA 371 biomarker is likely to change everything, including essentially upstaging clinical stage 1 patients with persistent miR371 expression and potentially doing RPLND in these patients, and potentially giving adjuvant chemotherapy to clinical stage 2 patients who have persistent miR371 expression after surgery.
To further validate the role of miR371 in clinical stage 2 germ cell tumor patients, Dr. Daneshmand showed the following clinical trial concept, which uses tumor size on imaging as well as miR371 expression to choose treatment and monitoring strategy.

He then went on to discuss the second study, which looked at detection and treatment outcomes of patients with late relapse germ cell tumors. Late relapse is defined as occurring more than 2 years after successful primary treatment and is slightly more common in non-seminoma (3.2% of all patients versus 1.4% of all seminoma patients). The timing of late relapse after year three is unpredictable, with a median of 7-10 years. Late relapses can be detected by symptoms, elevated tumor markers (more commonly AFP), or radiographic abnormalities. The most common site of late relapse is the retroperitoneum, less commonly the mediastinum (12%). The histology of relapse is often missed including teratoma, some germ cell components, as well as transformed components such as sarcoma and adenocarcinoma in a minority of cases. Salvage chemotherapy alone is ineffective at obtaining complete response, and surgery is, therefore, a critical treatment modality in late relapses. However, patients with chemotherapy-naïve disease and late relapse tend to be more chemotherapy sensitive. Patient education on signs and symptoms to watch out for, as well as continued surveillance, are key for the detection of late relapses.
Dr. Daneshmand ended with a summary slide from these two studies.

Presented by: Siamak Daneshmand, MD, Professor of Urology and Director of Urologic Oncology, University of Southern California, Los Angeles, USA
Written by: Alok Tewari, MD, PhD, Medical Oncologist at the Dana-Farber Cancer Institute, at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021


