The overall cohort of 90 patients is described below. Most patients had an initial non-seminoma of the testis, and the cohort was almost evenly split between chemotherapy-naïve and chemotherapy-exposed patients. Chemotherapy-exposed non-seminoma patients had a longer median time to late relapse relative to other groups of patients. Of the 42 chemotherapy-exposed patients, 6 had clinical stage 1 disease at diagnosis whereas 12 had stage 2 and 24 had stage 3 disease. Twenty-three out of 42 had IGCCCG good risk disease, with 9 and 10 patients having intermediate and poor-risk disease respectively. Of the chemotherapy-naïve late relapse patients, 43/48 were diagnosed with clinical stage 1 disease, 4 patients with stage 2, and 1 patient with stage 3 disease. All five patients with metastatic disease at diagnosis had good risk disease. Histologies of the non-seminoma patients were predominantly pure embryonal or mixed, with either yolk sac or teratoma next
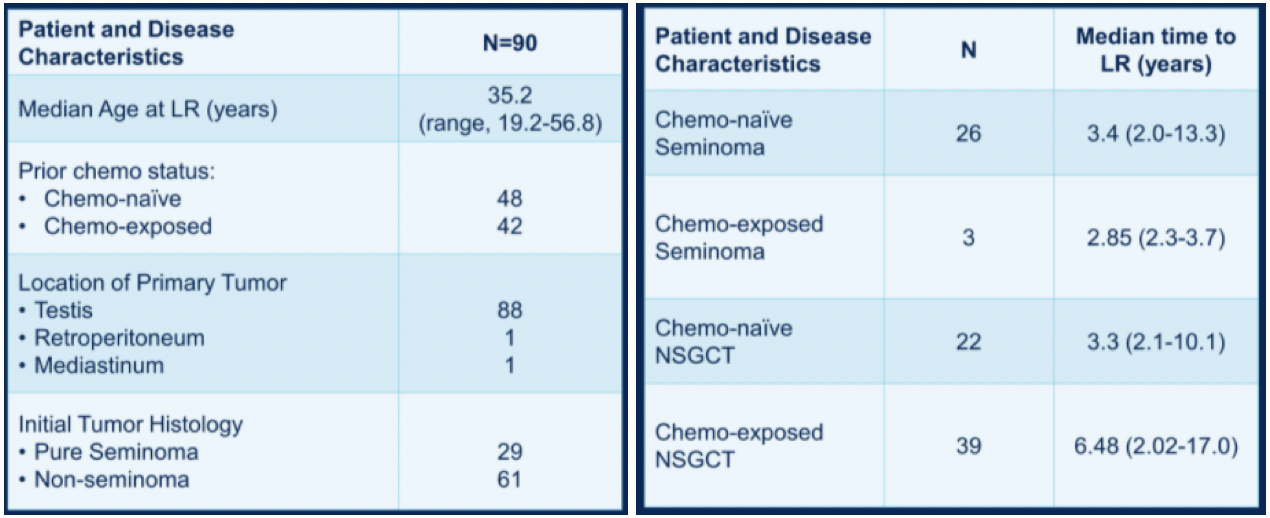
The timeframe of diagnosis of late relapse by chemotherapy exposure and histology is shown below. Most seminoma late relapses occurred by 5 years post-diagnosis, whereas more than half of chemotherapy-exposed non-seminoma late relapses occurred after five years.

Half of the relapses in the chemotherapy-naïve group were diagnosed by imaging, whereas more than half of the relapses in the chemotherapy-exposed group were detected initially by AFP level. Treatment of late relapses by chemotherapy exposure and histology are shown below.

At a median follow-up of just over three years since late-relapse diagnosis, chemotherapy-naïve patients have a statistically significant higher percentage of progression-free (70.1% vs 36.5%) and overall survival (97.4% vs 70.5%). Progression-free and overall survival data broken down by histology is shown below. Notably, chemotherapy-exposed non-seminoma had the lowest 2-year progression-free and overall survival amongst groups.

Of the 39 patients with prior chemotherapy exposure and nonseminoma, seven were treated with chemotherapy alone, thirteen with surgery alone, and nineteen with surgery and chemotherapy. No patients were free of progression if treated with chemotherapy alone, whereas almost half of patients treated with surgery or combination therapy were free of progression at two years.

The clinical status of patients in this cohort at last follow-up is shown in the table below.

Dr. Richardson concluded that patients diagnosed with germ cell tumors require lifelong follow-up with at least an annual physical with tumor markers. Chemotherapy exposure is associated with a different clinical course, and most chemotherapy-exposed late relapses are detected initially by elevated AFP. Surgical resection remains the preferred cornerstone of therapy for patients with chemotherapy-exposed late relapses (mostly non-seminoma in this cohort).
Presented by: Noah H. Richardson, MD, Resident in Internal Medicine at the Indiana University School of Medicine, Indianapolis, IN
Written by: Alok Tewari, MD, PhD, Medical Oncologist at the Dana-Farber Cancer Institute, at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021
References:
- David W. George, Richard S. Foster, Robert A. Hromas, et al. "Update on Late Relapse of Germ Cell Tumor: A Clinical and Molecular Analysis." Journal of Clinical Oncology. 2003. 21:1, 113-122.


