(UroToday.com) The 2023 American Society of Clinical Oncology (ASCO) annual meeting held in Chicago, IL between June 2nd and June 6th was host to an oligometastatic renal cell carcinoma (RCC) session. Dr. Shawn Dason discussed the role of cytoreductive nephrectomy and surgical metastatectomy in this setting.
Dr. Dason began with a case presentation of a 64-year-old female with an incidentally found 8 cm renal mass. On staging work-up with a CT scan, the patient was found to have a 2 cm rib lesion, that was biopsy-confirmed clear cell RCC. The patient was also found to have a single pulmonary metastatic lesion. Are there roles for surgery, systemic therapy, and/or radiotherapy in this setting?
While many definitions have been proposed, oligometastatic RCC commonly refers to those cases with up to five metastatic lesions at presentation. This group can be further divided into metachronous (prior nephrectomy) and synchronous (kidney in situ) subgroups.
There is limited data available to estimate the prevalence of oligometastatic RCC in clinical practice. Limited population-level data suggest that approximately 50% of RCC patients have single organ site metastases and about 25% of patients undergoing a nephrectomy are candidates for a complete metastasectomy.
Before considering patients for surgical therapy, we need to consider the patients’ International Metastatic RCC Database Consortium (IMDC) risk score, which is calculated based on:
- Karnofsky performance status <80%
- Time from diagnosis to systemic therapy <1 year
- Low hemoglobin level below the lower limit of normal
- High neutrophils count greater than the upper limit of normal (ULN)
- High platelets count greater than the ULN
- High corrected calcium level greater than the ULN
The IMDC risk grouping has been demonstrated to be strongly prognostic of overall survival (OS) outcomes in numerous studies. While originally developed in the era of vascular endothelial growth factor receptor tyrosine kinase inhibitors (VEGF-TKIs), a recent validation study in the Checkmate 214 cohort of patients receiving ipilimumab + nivolumab demonstrated that this risk stratification system remained strongly prognostic of OS outcomes.1
This was further validated in a recent publication from the IMDC consortium that demonstrated that IMDC risk grouping remained strongly prognostic for OS in patients receiving immune checkpoint inhibitor combination therapy, whether it was ICI dual therapy or ICI-VEGF combinations.
We note that IMDC risk grouping is not static and may change in the post-nephrectomy setting. Silagy et al. have demonstrated that an IMDC score improvement at 6 weeks post-nephrectomy is associated with improved survival outcomes as demonstrated in the Kaplan Meier curves below: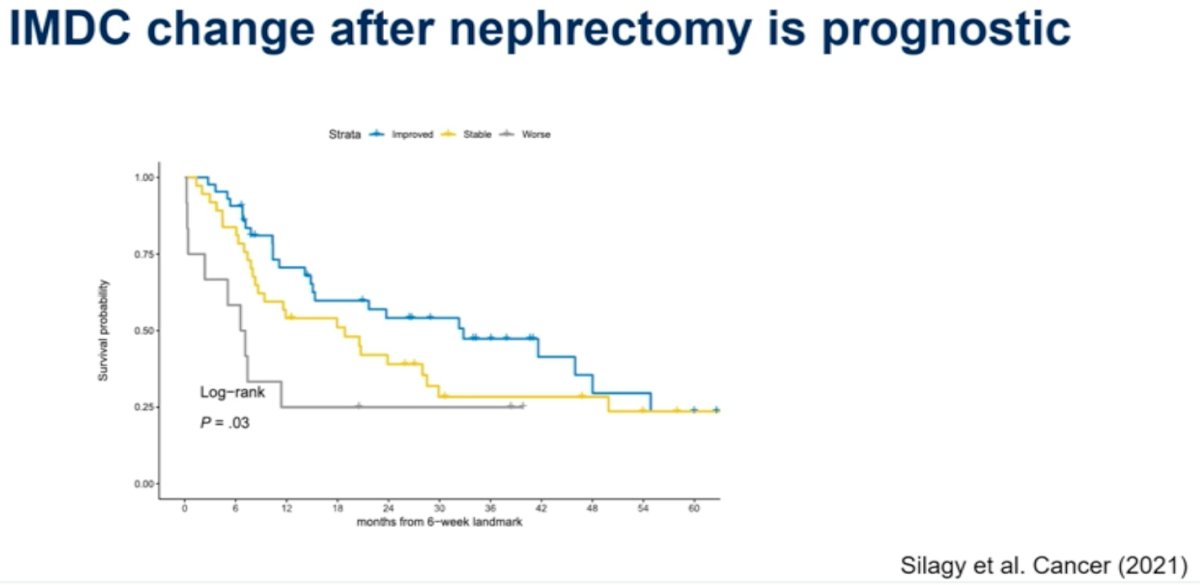
Cytoreductive nephrectomy refers to those surgeries performed in the setting of synchronous metastatic disease. Analysis of the NSQIP data between 2019 and 2021 demonstrates that the perioperative mortality and major complication rates are 1% and 8%, respectively. The median hospital length of stay following these procedures is 3 days (IQR: 2-5 days).
What is the current role of cytoreductive nephrectomy in the metastatic clear cell RCC setting? The ASCO guidelines suggest that cytoreductive nephrectomy be considered in select patients with one IMDC risk factor and for those who can have a significant majority of their tumor burden removed at the time of surgery (i.e., majority of disease is in the kidney).
Dr. Dason argued that a minimally invasive approach to these surgeries is favored with such approaches associated with lower levels of pain, shorter recovery times, short hospital length of stays (24 to 48 hours), and enhanced early recovery. It is also important to consider the timing of cytoreductive nephrectomy. With the improved response rates observed with ICI-combination systemic therapies, along with findings from SURTIME and CARMENA,3,4, there has been a gradual shift towards giving upfront systemic therapy and considering cytoreductive nephrectomies in the deferred early and late phases in responders.
When considering upfront nephrectomy, a key consideration should be the plan for the remaining disease sites, be it active surveillance, metastasis-directed therapy, or systemic therapy. What are some contraindications for cytoreductive nephrectomy?
- Significant extrarenal disease
- Excessive surgical morbidity
- Multiple IMDC risk factors
Why do the ASCO guidelines recommend considering cytoreductive nephrectomy for patients with only one IMDC risk factor. Evidence from the CARMENA trial, which randomized patients with metastatic clear cell RCC to either upfront cytoreductive nephrectomy followed by sunitinib versus upfront sunitinib followed by potential nephrectomy, as per investigator discretion (18% of patients in this arm), demonstrates that patients in the upfront cytoreductive nephrectomy arm with one IMDC risk factor had non-significantly prolonged overall survival (31 versus 25 months; p=0.2), whereas those with two or more IMDC risk factors had shorter survival with upfront cytoreductive nephrectomy (18 versus 31 months; p =0.03).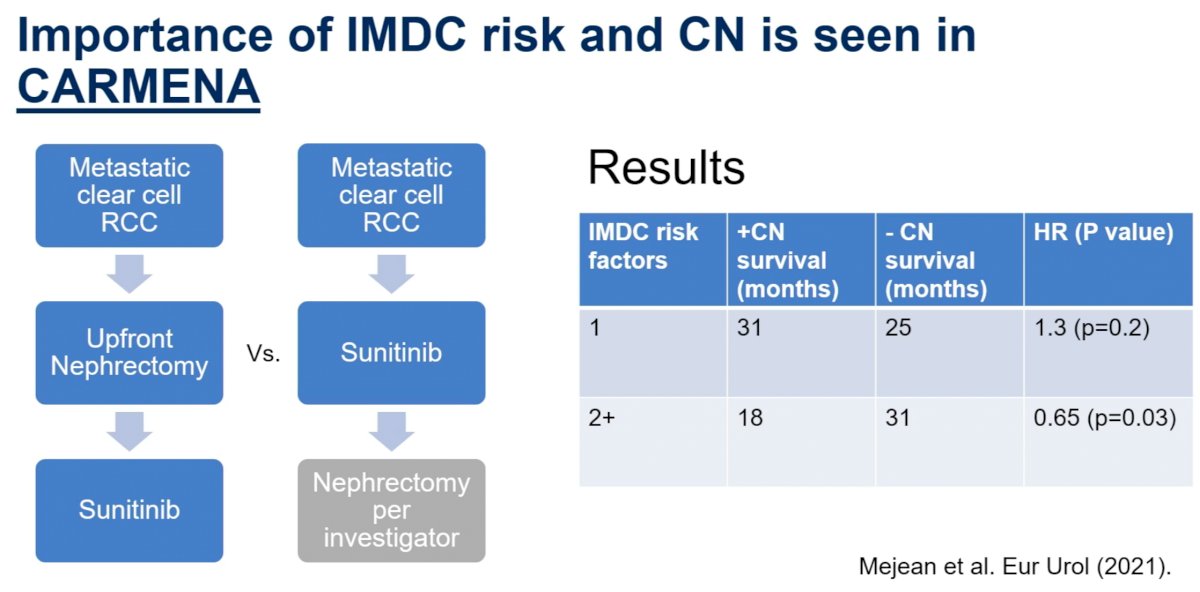
For surgical metastasectomy, population-level, administrative data demonstrate that these procedures are associated with perioperative mortality and major complication rates of 1% and 8%, respectively. The median hospital length of hospital stay with surgical metastasectomy is 4 days (IQR: 2 – 7 days). Increased complication rates are observed with older patients, those with multiple sites of resection, and those undergoing pancreatic resections.
What are the goals of complete metastasectomy?
- Delay systemic therapy
- Palliate symptoms
- Potentially prolong survival and improve quality of life
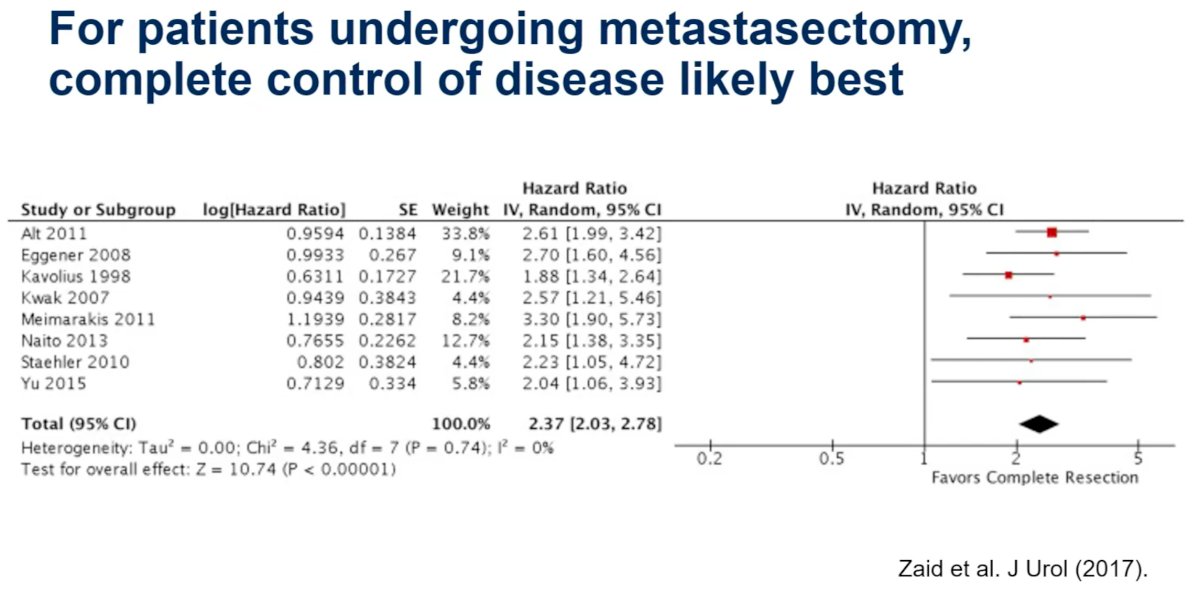
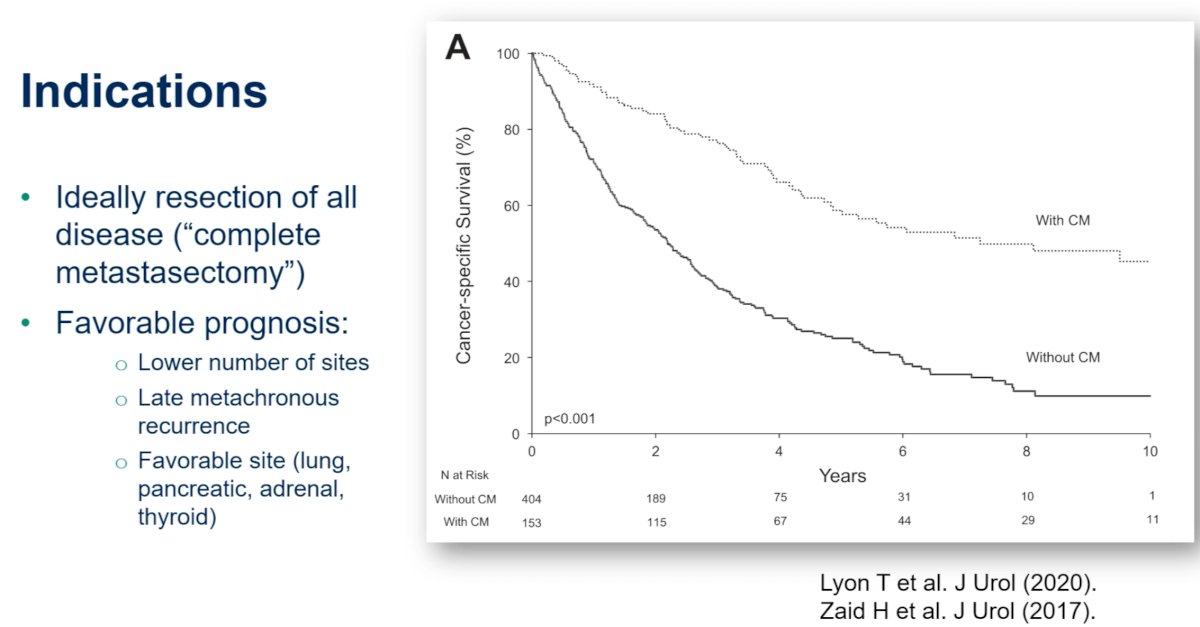
Aggregated evidence suggests that complete control of metastatic disease sites, where feasible, is associated with improved survival outcomes.
Dr. Dason concluded his presentation with the following take home messages for surgery in oligometastatic RCC:
- Consider upfront cytoreductive nephrectomy if patients have limited metastatic disease and are planned forr:
- Active surveillance of the metastatic sites
- Metastasis-directed therapy
- Systemic therapy and have no other IMDC risk factors
- Metastasectomy is best when “complete” with acceptable morbidity
Presented by: Shawn Dason, MD, Assistant Professor, Department of Urology, The Ohio State University Comprehensive Cancer Center, Columbus, OH
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, June 2 – Tues, June 6, 2023.
References:- Motzer R, McDermott DF, Escudier B, et al. Conditional survival and long-term efficacy with nivolumab plus ipilimumab versus sunitinib in patients with advanced renal cell carcinoma. Cancer, 2022;128(11):2085-2097.
- Ernst MS, Navani V, Wells JC, et al. Outcomes for International Metastatic Renal Cell Carcinoma Database Consortium Prognostic Groups in Contemporary First-line Combination Therapies for Metastatic Renal Cell Carcinoma. Eur Urol, 2023;S0302-2838(23)00001-5.
- Mejean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal cell carcinoma. N Engl J Med, 2018 2;379(5):417-427.
- Bex A, Mulders P, Jewett M, et al. Comparison of immediate vs deferred cytoreductive nephrectomy in patients with synchronous metastatic renal cell carcinoma receiving sunitinib: The SURTIME Randomized Clinical Trial. JAMA Oncol, 2019;5(2):164-170.


