(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) annual meeting held in Chicago, IL between May 31 and June 4 was host to the Session: Managing Variant Histologies in Urothelial and Renal Cell Cancers. Dr. Eva Katharina Masel talked about the considerations in treating and palliating variant Genitourinary Cancers where no standard of care exists.
Dr. Masel began her presentation by saying palliative care is not just about end-of-life care; it's about living in the best possible way with the disease. Palliative care professionals aim to be seen as a lighthouse, guiding patients through the storms that may come.
She continues by drawing a parallel between trauma care and palliative medicine. Just as trauma care follows the ABCDE approach (Airway, Breathing, Circulation, Disability, Expose), palliative medicine utilizes the ABCD approach, which stands for Attitude, Behavior, Compassion, and Dialogue. This framework applies across all areas of medicine. Regardless of a patient's age or health condition, the core values of kindness, respect, and dignity remain indispensable. This approach serves as a reminder to practitioners about the importance of both caring for and caring about their patients. (1)
Palliative care can be defined as specialized healthcare focused on improving quality of life for patients with serious illnesses and can aid other clinicians in addressing patients' unmet symptoms, coping mechanisms, and communication needs. The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN). guidelines recommend integrating palliative care into standard oncological treatment based on multiple randomized trials demonstrating significant improvements in physical well-being, patient satisfaction, and goal-concordant care. (2) It is crucial to understand the need for a palliative care consultation when caring for cancer patients, Dr Masel mentioned 7 indications that we should keep in our minds for a timely referral to palliative medicine:
- High health care resource utilization
- Persistent pain or high risk of poor pain management
- High non-pain symptom burden or symptoms refractory to initial management
- Limited anticancer treatment options
- Need for advanced communication skills
- Complex patient and/or caregiver circumstances
- Oncology care team challenges
Referrals to palliative care often occur in the late and advanced stages of the disease, leading to untreated symptoms, patient distress, and unnecessary aggressive treatments at the end of life. One major barrier to early referrals is the common association of palliative care with hopelessness, cessation of cancer treatment, and death. Although physicians may explain the benefits of early palliative care, overcoming patients’ negative preconceptions can be challenging. To help facilitate these conversations, the metaphor "Palliative Care Is the Umbrella, Not the Rain" can be used in clinical practice. This metaphor helps guide discussions in advanced cancer, making patients more open to seeing a palliative care specialist. (3)
Dr. Masel discussed the importance of communication with cancer patients and introduced another framework: CARE, which stands for Communicate, Advocate, Respect, and Empathize. Briefly, this means we should communicate warmly and welcomingly with patients, advocate on behalf of patients, families, colleagues, and ourselves, respect and embrace differing values, opinions, and viewpoints, and empathize with and acknowledge the feelings of others.
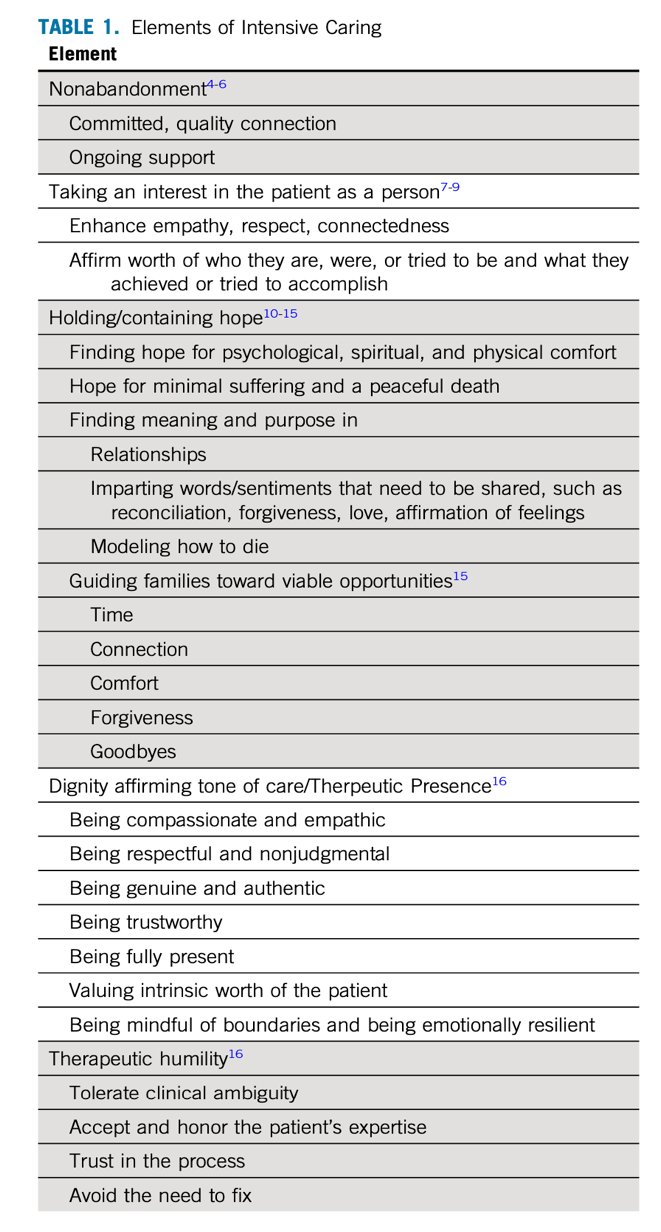
There is abundant evidence that patients nearing the end of life often feel they no longer matter. This sense of burden can affect both the patients, who may feel like a burden to others, and their family members, who may feel helpless and exhausted, reinforcing the patients' feelings of burden. Intensive caring involves finding ways to remind patients that they still matter. A foundational element of this approach is non-abandonment, which requires committed, ongoing care and compassion, even when patients no longer care about themselves. The assurance of continued support and care is crucial in helping patients feel valued. The elements of intensive caring are illustrated in the table below:
As physicians caring for cancer patients, we often tend to distance ourselves from palliative care. This behavior is akin to the phenomenon in nature known as "crown shyness," where a tree's leaves withdraw from the leaves of other trees. Instead, we should avoid this distancing and work together as a team to improve the care of our cancer patients.
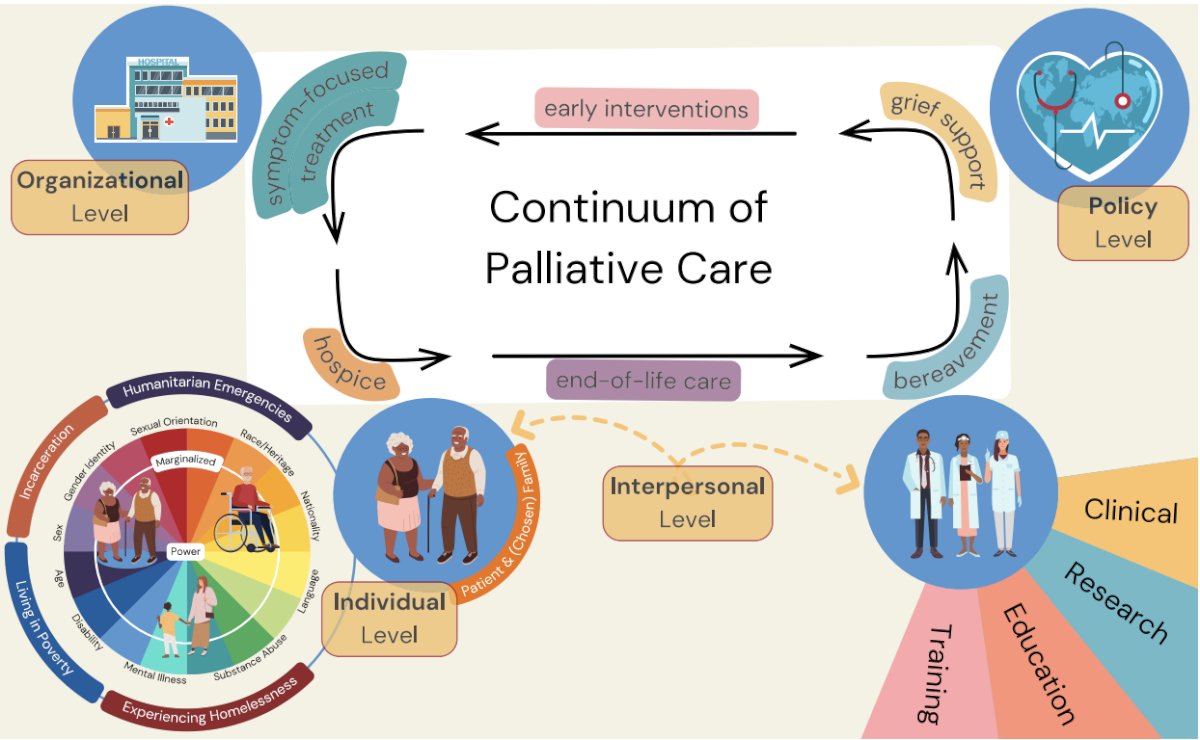
Dr Masel went on to discuss the continuum of palliative care, this implies that to improve equity and inclusivity in palliative care we have to follow an individual-centered strategy endorsed by the community and promoting change across various fronts:
- Individual (patient and caregiver)
- Interpersonal (health care team)
- Organizational
- At the policy level
Ensuring fair access is essential throughout the entire spectrum of palliative care services, starting from early interventions and extending to symptom-focused treatment, hospice care, end-of-life support, and bereavement assistance. The continuum of care is illustrated in the figure below.(5)
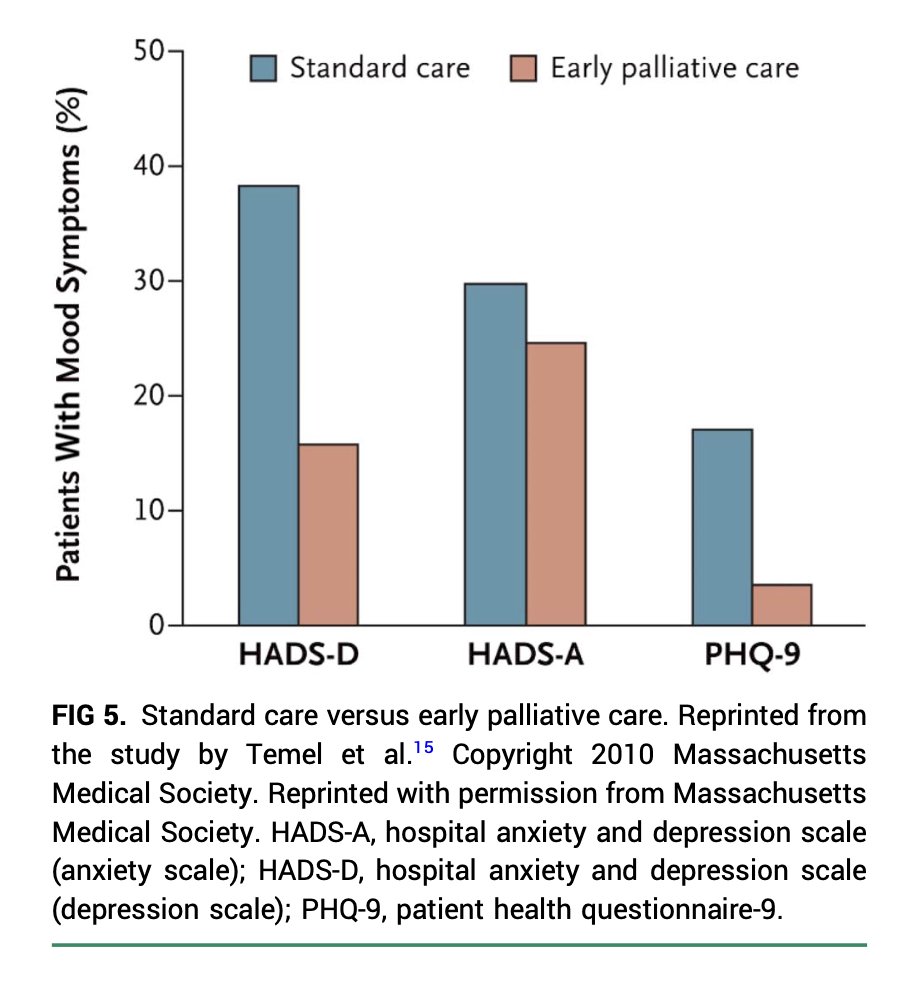
Dr. Masel discussed a randomized clinical trial published in 2010 involving patients newly diagnosed with metastatic non-small-cell lung cancer. Participants were allocated to receive either early palliative care integrated with standard oncologic care or standard oncologic care alone. Results showed that those assigned to early palliative care demonstrated a better quality of life compared to those receiving standard care. Additionally, fewer patients in the early palliative care group exhibited depressive symptoms, as assessed by the Hospital Anxiety and Depression Scale (HADS-D, HADS-A) and the Patient Health Questionnaire-9 (PHQ-9) (6).
Finally, the palliative care intervention should be directed to:
- Illness understanding/education
- Inquire about illness and prognostic understanding
- Offer clarification of treatment goals
- Symptom management
- Inquire about uncontrolled symptoms, referral or prescriptions, if necessary
- Mode of decision making
- Assist with treatment decision-making, if necessary
- Coping with life threatening illness
- Patients and caregivers
Dr Masel wrapped up her presentation with following key messages:
- Palliative Care Is the Umbrella, Not the Rain
- We have to improve our communication, this is a clinical skill and words matter
- It is not either or, but both - Oncology and Palliative Care
- How people die remains in the memory of those who live on
Presented By: Eva Katharina Masel, MD, PhD, Full Professor and Head of the Clinical Division of Palliative Care at the Medical University of Vienna
Written By: Julian Chavarriaga, MD – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, May 31 – Tues, June 4, 2024
References:
- Chochinov HM. Dignity and the essence of medicine: the A, B, C, and D of dignity conserving care. BMJ. 2007 Jul 28;335(7612):184-7. doi: 10.1136/bmj.39244.650926.47. PMID: 17656543; PMCID: PMC1934489.
- Hugar LA, Wulff-Burchfield EM, Winzelberg GS, Jacobs BL, Davies BJ. Incorporating palliative care principles to improve patient care and quality of life in urologic oncology. Nat Rev Urol. 2021 Oct;18(10):623-635. doi: 10.1038/s41585-021-00491-z. Epub 2021 Jul 26. PMID: 34312530; PMCID: PMC8312356.
- Zimmermann C, Mathews J. Palliative Care Is the Umbrella, Not the Rain-A Metaphor to Guide Conversations in Advanced Cancer. JAMA Oncol. 2022 May 1;8(5):681-682. doi: 10.1001/jamaoncol.2021.8210. PMID: 35297961.
- Chochinov HM. Intensive Caring: Reminding Patients They Matter. J Clin Oncol. 2023 Jun 1;41(16):2884-2887. doi: 10.1200/JCO.23.00042. Epub 2023 Apr 19. PMID: 37075272; PMCID: PMC10414729.
- Koffman J, Shapiro GK, Schulz-Quach C. Enhancing equity and diversity in palliative care clinical practice, research and education. BMC Palliat Care. 2023 Jun 5;22(1):64. doi: 10.1186/s12904-023-01185-6. PMID: 37271813; PMCID: PMC10239712.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010 Aug 19;363(8):733-42. doi: 10.1056/NEJMoa1000678. PMID: 20818875.


