(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) Annual Meeting held in Chicago, IL was host to a diagnostic and therapeutic strategies in renal cell carcinoma (RCC) state-of-the-art session. Dr. Shankar Siva discussed the integration of functional imaging in RCC focusing on the evidence and utility for functional imaging using PET scanning for:
- Patients with localized disease
- Patients with advanced disease
- Response assessment
- Future directions
Currently, triphasic CT or MRI with IV contrast remains the standard of care imaging approach for characterizing primary RCC lesions. Chest CT is recommended to rule out metastatic lung disease in patients at high-risk for tumor spread. Similarly, a bone scan, despite limitations in RCC, and CT or MRI brain are recommended in the presence of clinical symptoms suggestive of metastatic disease. Functional imaging, such as positron emission tomography (PET/CT) is not yet recommended in RCC by consensus guidelines.

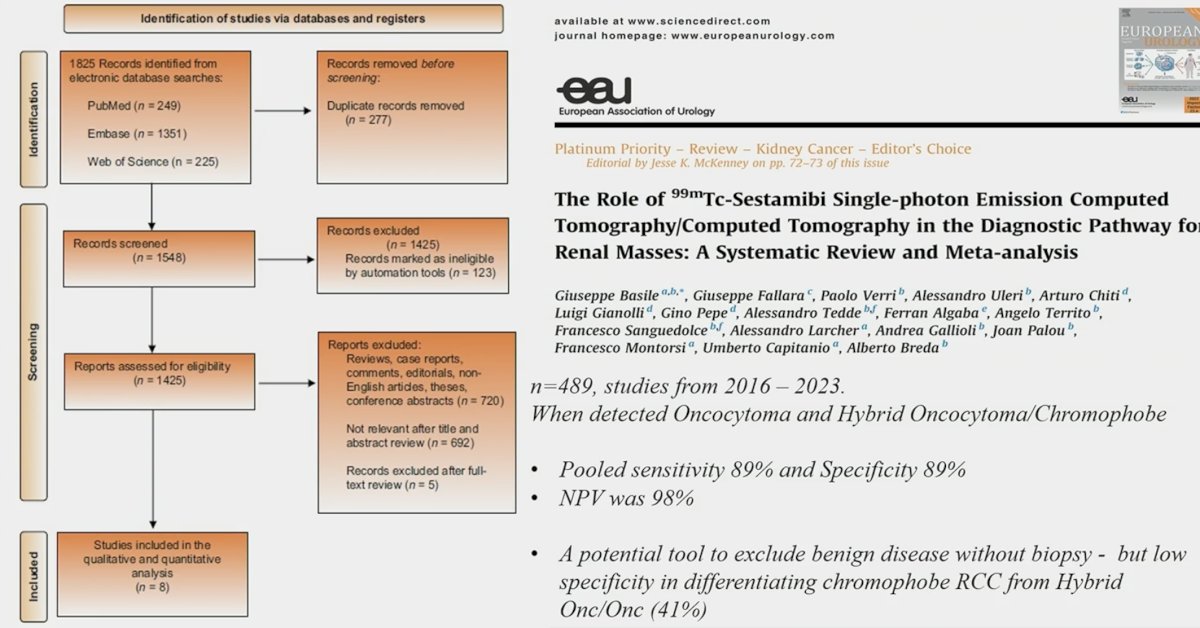
99mTechnetium-Sestamibi scan has long been employed in practice to better characterize indeterminate renal masses by differentiating renal oncocytoma and hybrid oncocytic/chromophobe tumors from all other renal lesions, including malignant subtypes. A 2024 meta-analysis of eight studies involving 489 patients with 501 renal masses demonstrated that the sensitivity and specificity of Sestamibi SPECT/CT for renal oncocytoma and hybrid oncocytic/chromophobe tumors, versus all other renal lesions, was 89% each. Notably, for renal oncocytoma and hybrid oncocytic/chromophobe tumors versus clear cell RCC and papillary RCC, Sestamibi SPECT/CT showed a specificity of 98% and similar sensitivity. As such, Sestamibi SPECT/CT is a potential tool to exclude benign disease without biopsy, but there was low specificity in differentiating chromophobe RCC from hybrid oncocytic/oncocytic tumors (41%).1
At ASCO GU 2023, Schuch et al. presented the results of the ZIRCON trial, which evaluated the diagnostic performance of 89Zr-DFO-girentuximab (TLX250-CDx) PET/CT. ZIRCON was an open-label, multicenter clinical trial. Patients with indeterminate renal masses (≤ 7 cm; tumor stage cT1) who were scheduled for a partial or radical nephrectomy within 90 days from planned 89Zr-DFO-girentuximab administration were eligible. Enrolled patients received a single dose of 89Zr-DFO-girentuximab (37 MBq ± 10%; 10 mg girentuximab) on Day 0 and underwent PET/CT imaging on Day 5 (± 2 days) prior to surgery:
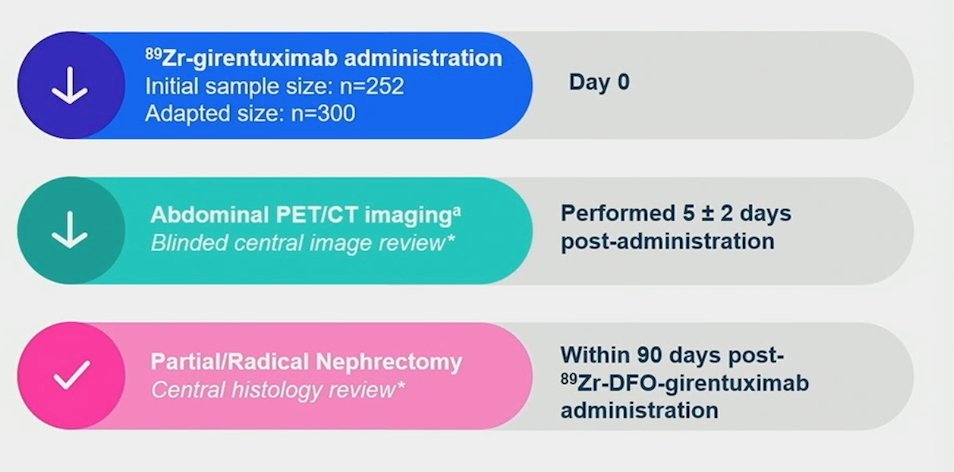
This imaging modality demonstrated:
- Sensitivity: 86%
- Specificity: 87%
- Positive predictive value: 91%
- Negative predictive value: 74%
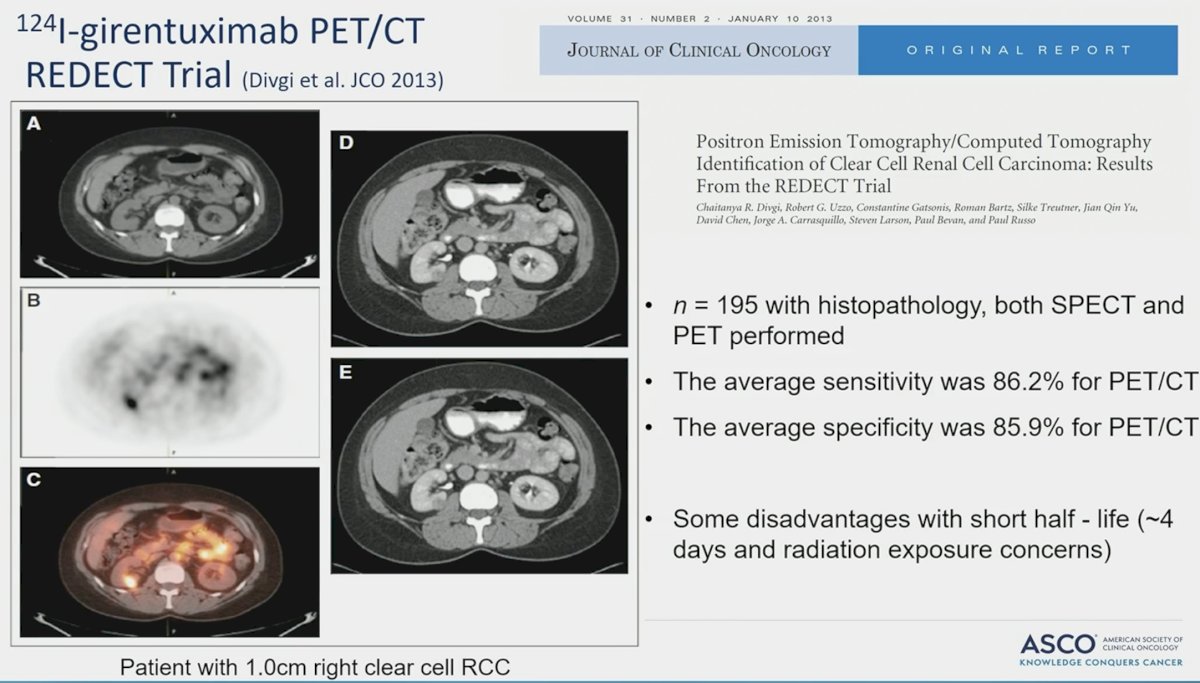
In 2013, Divgi et al. published the results of an open-label multicenter study of iodine-124 ((124)I) -girentuximab PET/CT in patients with renal masses who were scheduled for resection. PET/CT and contrast-enhanced CT (CECT) of the abdomen was performed 2 to 6 days after intravenous (124)I-girentuximab administration and before resection of the renal mass(es). The average sensitivity of PET/CT was 86% (versus 76% for CECT) and the specificity was 86% (versus 47% for CECT). This study represented the first clinical validation of a CAIX-targeting radiotracer for PET/CT imaging for the accurate and non-invasive identification of clear cell RCC.2
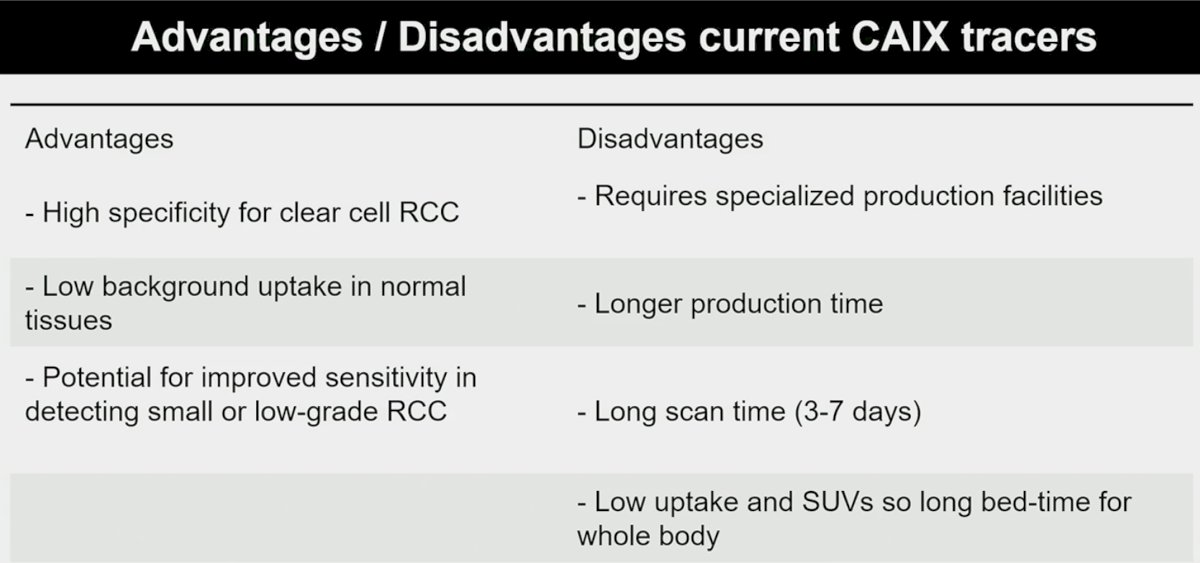
What are some advantages/disadvantages for current CAIX tracers?
PSMA-targeted imaging has also emerged in the metastatic RCC setting. However, in contrast to prostate cancer, where PSMA (prostate-specific membrane antigen) is expressed on the cancerous cell surface, PSMA is not expressed by conventional RCC tumor cells. It is instead expressed in the renal neovasculature.

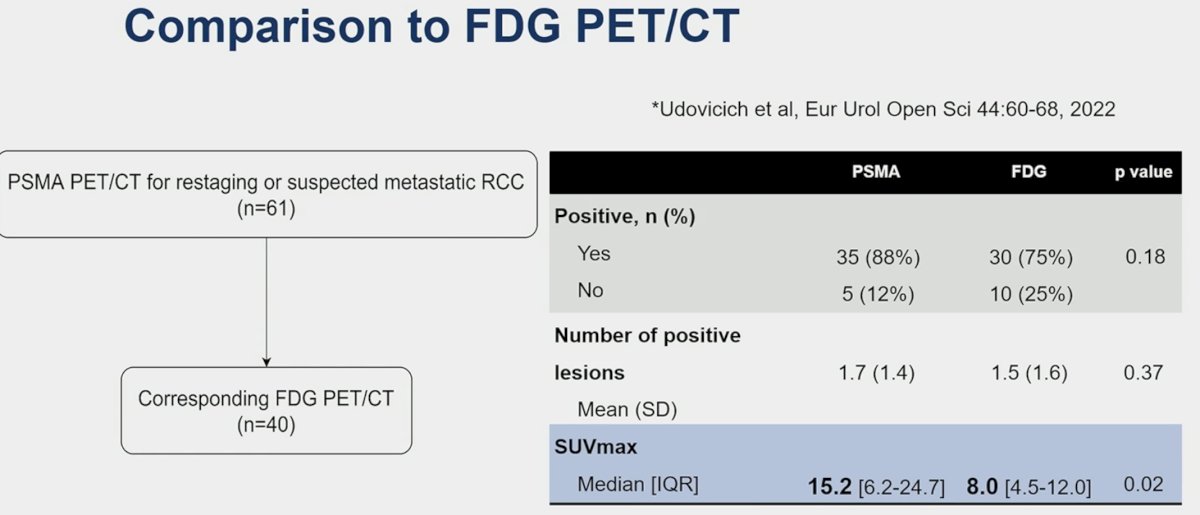
In 2022, Dr. Siva’s group published the results of a retrospective review of 61 patients (54 clear cell RCC) who underwent PSMA PET/CT from 2014 to 2020 for restaging or suspected metastatic RCC at a tertiary academic setting. PSMA-positive disease was detected in 51 patients (84%). For 30 patients (49%) there was a change in management due to PSMA PET/CT (high impact, 29 patients, 48%). In 15 patients (25%), more metastases were detected on PSMA PET/CT than on CT. The sensitivity of combined PSMA PET/CT and diagnostic CT was 91%. In a subcohort of 40 patients, the detection rate was 88% for PSMA and 75% for FDG PET/CT (p=0.17). 70% of patients had PSMA+/FDG+ concordance, whereas 18% had PSMA+/FDG- discordance.3

What are the advantages/disadvantages of PSMA PET in RCC?
- Advantages
- High sensitivity for detecting clear cell RCC
- Ability to detect metastases
- Potential for guiding treatment decisions/management impact
- 68Ga can be produced on-site, with rapid scan time
- Disadvantages
- Not good for renal primary
- Slow at response assessment compared to FDG
- Higher cost compared to other imaging modalities
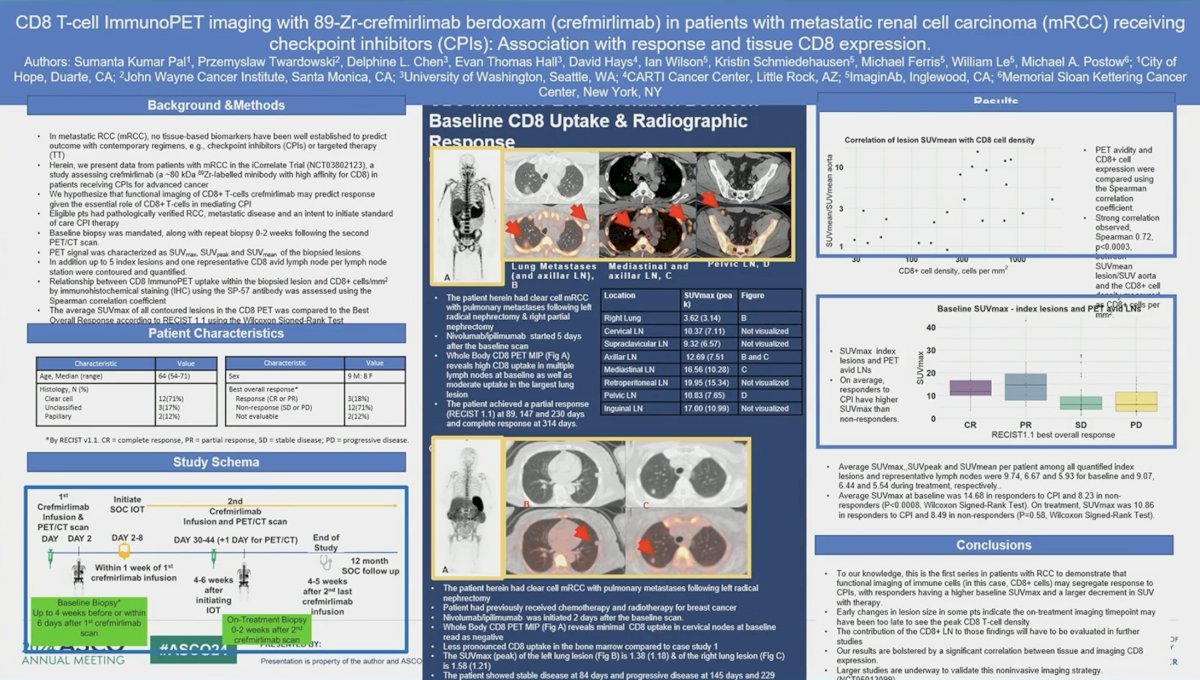
What are the future directions in this space? Dr. Siva highlighted a poster being presented at this meeting investigating CD8 T-cell ImmunoPET imaging with 89-Zr-crefmirlimab berdoxam (crefmirlimab) in patients with metastatic (mRCC) receiving checkpoint inhibitors:
Other radiotracers being evaluated in this setting include [68Ga]Ga-DPI-4452, a novel CAIX PET tracer.
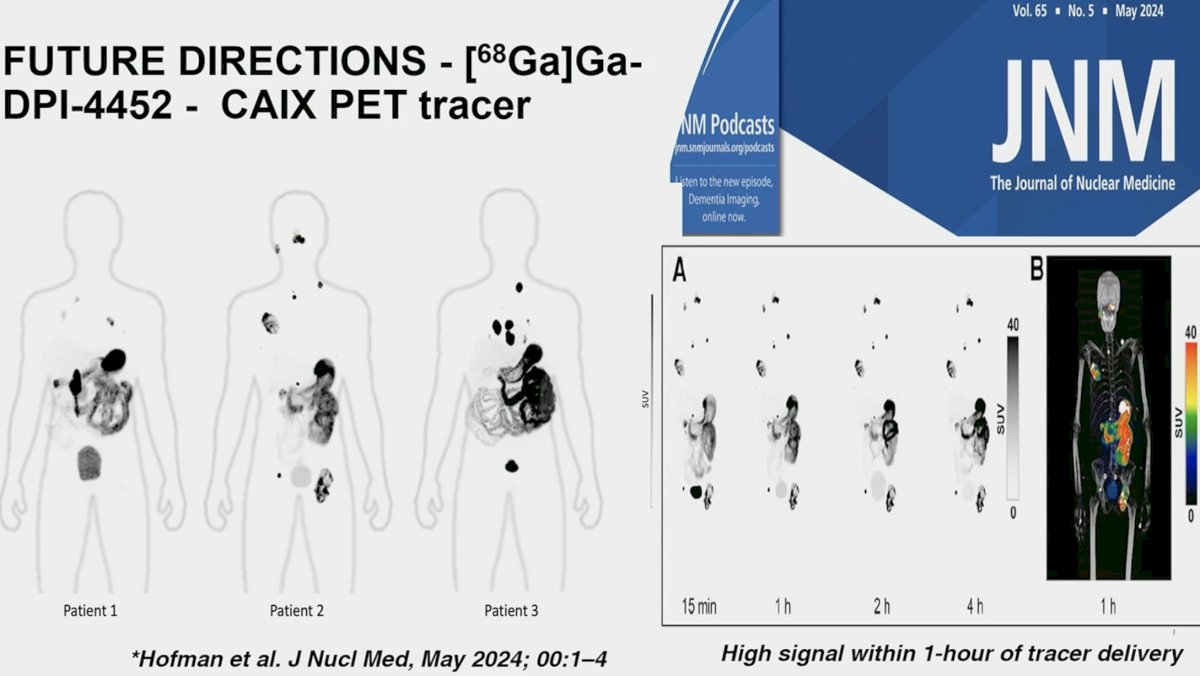
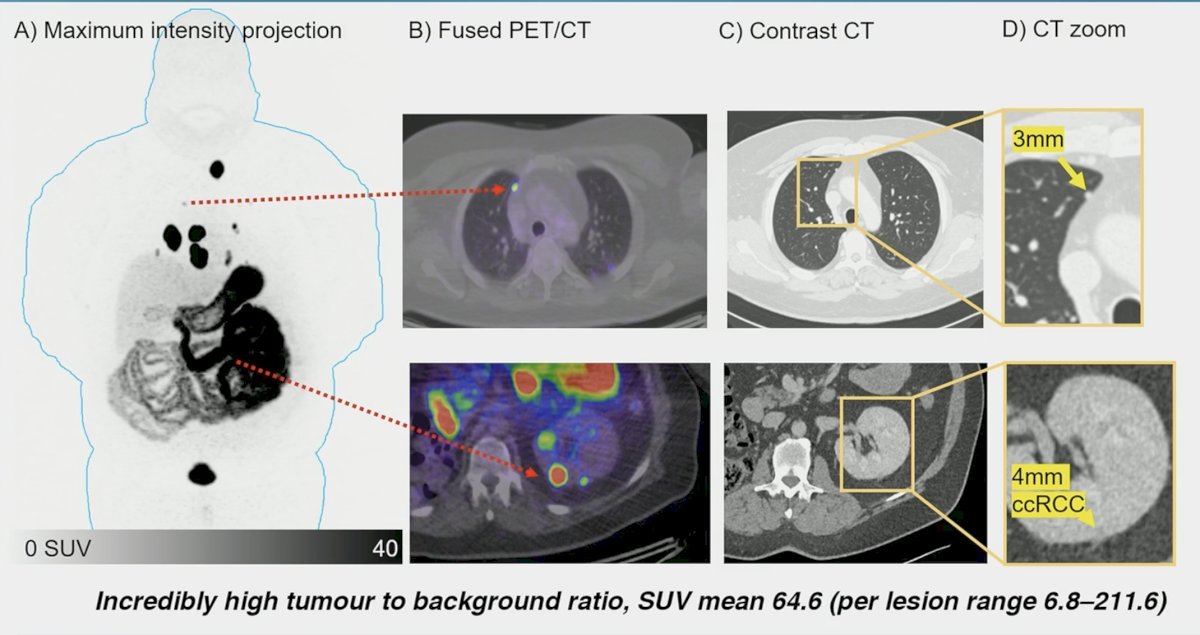
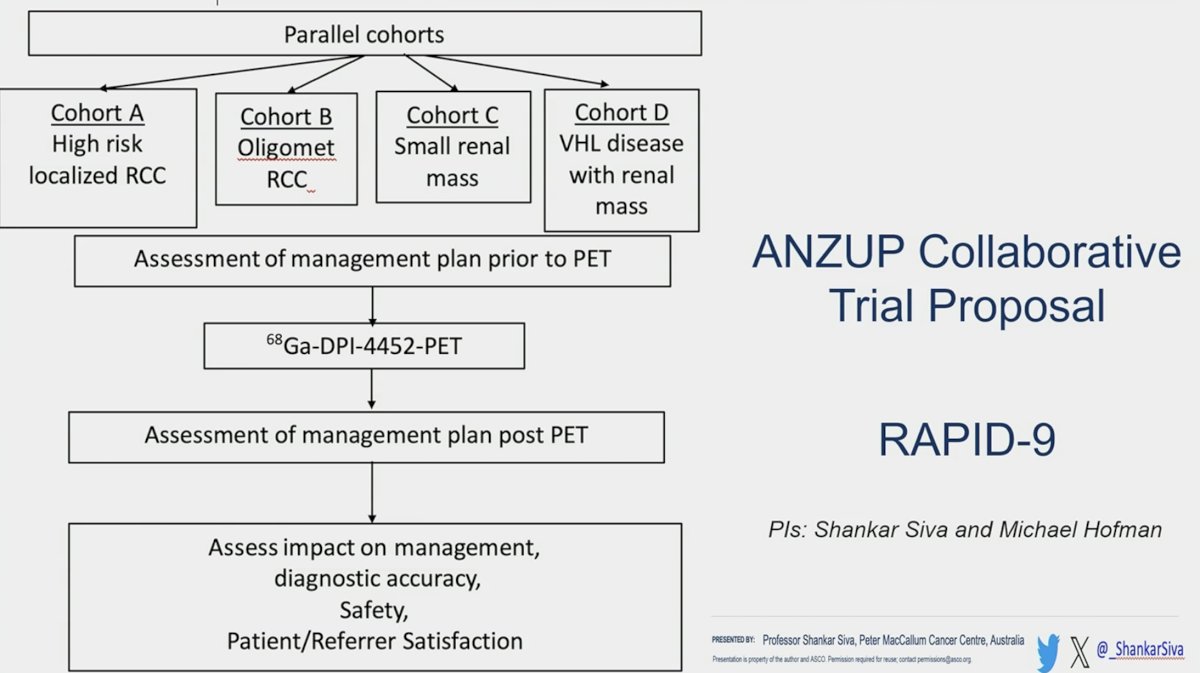
The RAPID-9 ANZUP Collaborative trial is evaluating 68Ga-DPI-4452-PET in RCC patients (high-risk localized, oligometastatic, small renal masses, VHL disease with renal mass) and its impact on treatment decision making, along with its diagnostic accuracy, safety, and patient/referrer satisfaction.
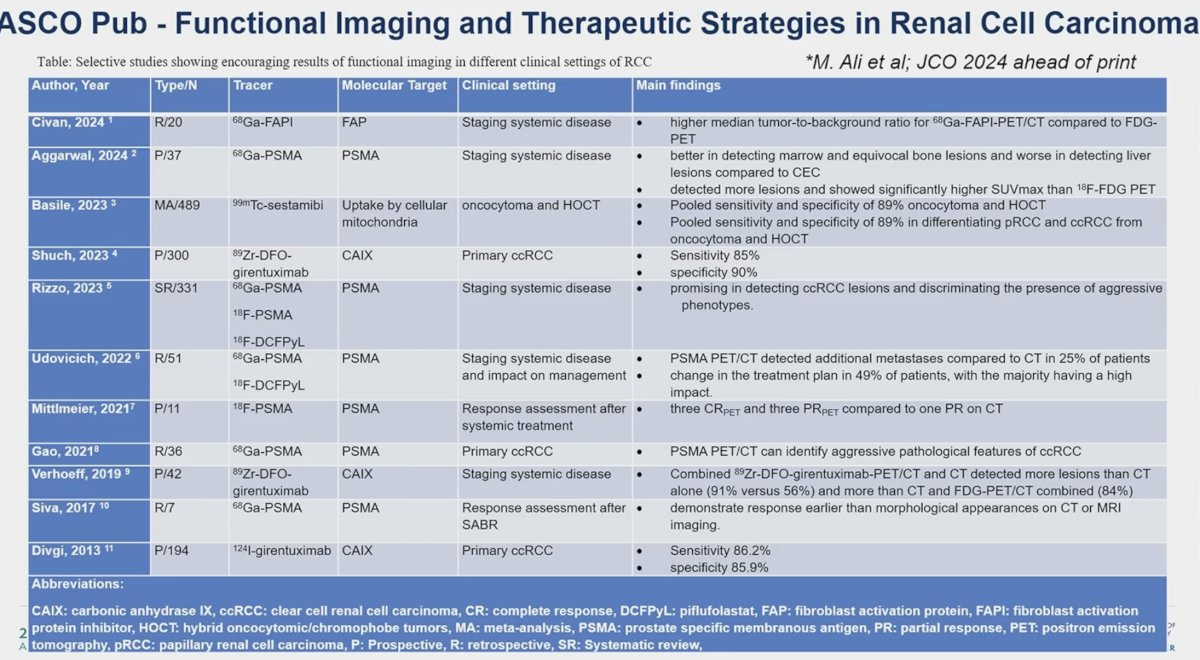
Dr. Siva provided an overview of the current functional imaging and therapeutic strategies in RCC:
He concluded by noting that functional imaging with PET is not yet standard of care. Functional imaging tools that are under evaluation and hold the greatest promise in this space, include:
- Localized disease
- Sestamibi, girentuximab
- Advanced disease
- PSMA PET, CA-IX tracers
- Response assessment
- FDG and PSMA PET
Presented by: Shankar Siva, PhD, MBBS, FRANZCR, Associate Professor, Peter MacCallum Cancer Centre, Melbourne, Australia
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, May 31 – Tues, June 4, 2024.
Related content: Functional Renal Imaging and Advances in Kidney Cancer Detection - Shankar Siva
References:
- Basile G, Fallara G, Verri P, et al. The Role of 99mTc-Sestamibi Single-photon Emission Computed Tomography/Computed Tomography in the Diagnostic Pathway for Renal Masses: A Systematic Review and Meta-analysis. Eur Urol. 2024;85(1): 63-71.
- Divgi CR, Uzzo RG, Gatsonis C, et al. Positron emission tomography/computed tomography identification of clear cell renal cell carcinoma: results from the REDECT trial. J Clin Oncol. 2013;31(2): 187-94.
- Udovicich C, Callahan J, Bressel M, et al. Impact of Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography in the Management of Oligometastatic Renal Cell Carcinoma. Eur Urol Open Sci. 2022;44: 60-8.


