(UroToday.com) The 2024 American Society of Clinical Oncology (ASCO) annual meeting featured a session on prostate cancer, and a presentation by Dr. Simon Crabb discussing the results of MANCAN2, a multicenter randomized controlled trial of self-help cognitive behavioral therapy to manage hot flush and night sweat symptoms in patients with prostate cancer receiving ADT.
Up to 80% of patients receiving ADT suffer hot flush and night sweats, which impacts quality of life and potentially ADT compliance. Hot flush and night sweats are associated with sleep disturbance, anxiety, low mood, and cognitive impairment. Non-pharmacological mitigation options lack adequate prospective data, Prior research has found self-help cognitive behavioral therapy, with minimal guidance, reduced hot flush, and night sweats due to ADT at 6 weeks. In breast cancer, cognitive behavioral therapy delivered by specialist nurses improved hot flush and night sweats impact at 6 months, in addition to sleep, anxiety, and depression scores. Dr. Crabb and colleagues tested the longer-term impact of self-help cognitive behavioral therapy, guided and delivered by prostate cancer nurse specialist teams.
MANCAN2 is a multicenter randomized controlled trial and process evaluation within UK prostate cancer units. Eligibility included:
- Localized/advanced prostate cancer
- On ADT with ≥ 6 months further planned
- Hot flush and night sweat problem rating scale ≥ 2
Patients were randomized (1:1) in groups of 6 to 8 to treatment as usual or cognitive behavioral therapy + treatment as usual, by permuted block, stratified by site, cohort, and treatment intent. The trial design for MANCAN2 is as follows: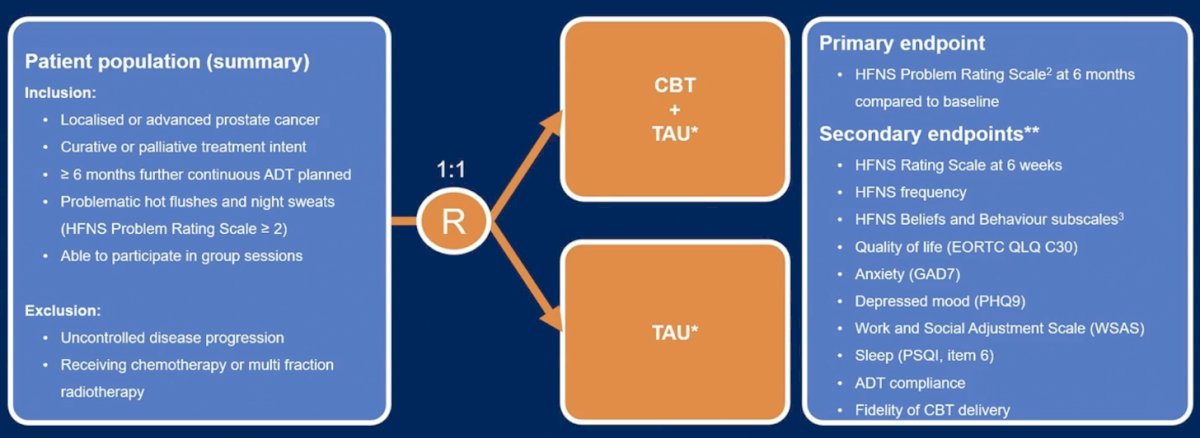
Cognitive behavioral therapy was a 4-week self-help intervention (booklet and relaxation audio) with pre- and post-intervention group workshops by the prostate cancer nurse specialist team:
The primary objective was assessing whether adding cognitive behavioral therapy to treatment, as usual, reduces the 6-month hot flush and night sweat problem rating scale versus baseline (mixed linear regression). Secondary endpoints included 6-week hot flush and night sweat problem rating scale, hot flush and night sweat frequency, hot flush and night sweat beliefs and behaviors, quality of life (EORTC QLQ-C30, symptoms (rating scales for anxiety, depression, mood, and sleep) by mixed logistic regression), and ADT compliance (chi-squared test). A 6-month mean hot flush and night sweat problem rating scale difference of ≥ 1.5 points was deemed clinically relevant and required data from 111 patients (90% power, 5% type 1 error, 6 to 8 patients per group, intra-class correlation 0.01, anticipating 26% patient loss).
There were 162 patients randomly assigned (81 per arm) and 117 returned 6-month hot flush and night sweat problem rating scale data. Baseline characteristics were balanced, and mean cognitive behavioral therapy delivery adherence was 85%: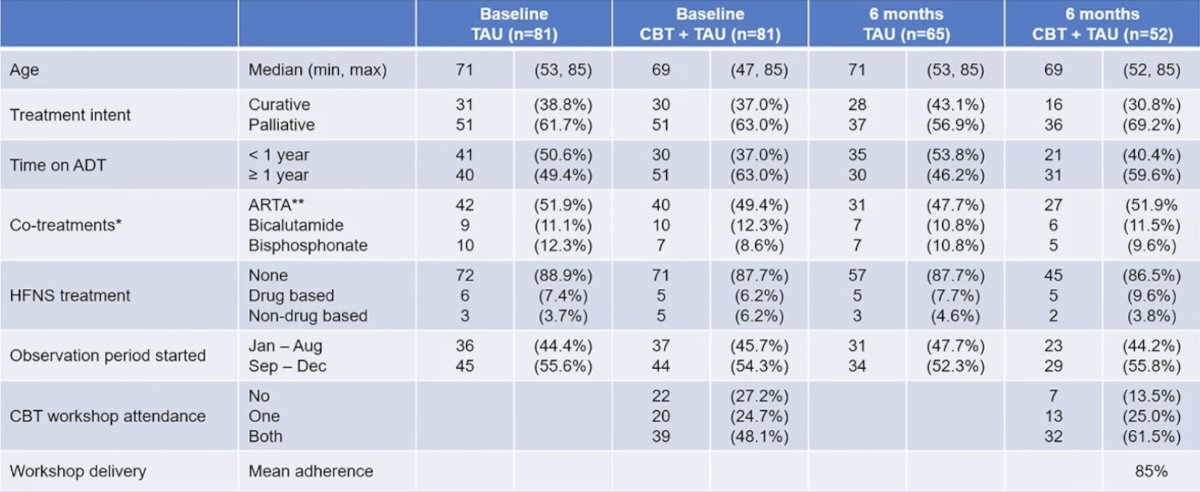
The 6-month mean hot flush and night sweat problem rating scale score was not significantly different for the treatment as usual alone versus cognitive behavioral therapy + treatment as usual (mean 4.08 vs 4.04, 95% CI for difference: -0.89, 0.80; p = 0.97), although a difference was observed at 6 weeks (mean 4.47 vs 3.79, 95% CI: -1.26, -0.09; p = 0.03):
At 6 weeks, cognitive behavioral therapy patients had a higher weekly hot flush and night sweat frequency (median 54.2 vs 59.4, 95% CI: 0.22, 10.19; p = 0.04), lower depression score (median 7.19 vs 6.19, 95% CI: -1.88, -0.12; p = 0.03) and lower anxiety score (median 4.25 vs 3.39, 95% CI: -1.64, -0.08; p=0.03). Cognitive behavioral therapy patients had more positive beliefs about openness and humor scores at 6 months (median 4.92 vs 4.59, 95% CI: -0.63, -0.03; p = 0.03). There was no significant difference for other measures of hot flush and night sweat beliefs and behaviors, quality of life, anxiety, mood, sleep quality, and treatment compliance. This trial also assessed compliance of ADT at 6 months, which showed 86% compliance in the treatment as-usual arm and 100% in the cognitive behavioral therapy arm (p = 0.006).
Dr. Crabb concluded his presentation discussing results from MANCAN2 with the following take-home messages:
- MANCAN2 confirms that a 4-week cognitive behavioral therapy intervention program, during ADT for prostate cancer, reduces the impact of hot flushes and night sweats at 6 weeks
- Anxiety and depression scores were also improved at this time point
- However, a difference in these effects was not seen at 6 months
- Further research should address the durability of the impact of cognitive behavioral therapy
- Training of existing prostate cancer nurse specialist teams to guide self-help cognitive behavioral therapy was viable
- 14% of the control arm patients discontinued ADT by 6 months compared to none for cognitive behavioral therapy. Further research should investigate the potential for cognitive behavioral therapy to support treatment compliance
Presented by: Simon J. Crabb, MD, Professor, University of Southampton and University Hospital Southampton NHS Foundation Trust, Southampton, UK
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, Fri, May 31 – Tues, June 4, 2024.


